PRESERVE gets to the heart of IVC filters
The new PRESERVE study (Predicting the Safety and Effectiveness of Inferior Vena Cava Filters) seeks to examine the best use of IVC filters by focusing on safety endpoints. The 5-year, multispecialty, prospective study will enroll approximately 1,800 patients who have inferior vena cava (IVC) filters placed at 50 U.S. facilities. The goal of investigators is to keep in contact with patients every 6 months with phone calls, clinical exams, and repeat imaging. Anyone who has a filter removed will be followed for 3 months.
The primary safety endpoints will be freedom from perforation, migration, embolization, deep vein thrombosis (DVT), or fatal pulmon- ary embolism (PE). Secondary endpoints include procedural complications, insertion site, DVT, or any other major complication including death or PE. Investigators hope to begin PRESERVE this year.
"This study is going to bring the care of people with venous thromboembolic disease under a magnifying glass and actually figure out the safety and efficacy of these filters," said Dr. Matthew Johnson, one of the PRESERVE study directors.
After the Food and Drug Administration (FDA) issued its 2010 safety communication on retrievable IVC filters, the Society for Vascular Surgery (SVS) and the Society of Interventional Radiology (SIR) convened a task force to study the issue. SVS and SIR formed the IVC Filter Study Group Foundation, a collaborative body to oversee the study – underscoring this paradigm-shifting, collaborative undertaking.
Citing 921 device adverse events, FDA urged follow-up with patients who had the filters and for physicians to consider removing the devices based on the individual risk/benefit ratio. The problem, FDA said, was not inherent in the filters themselves, but more "related to a retrievable filter remaining in the body for long periods of time, beyond the time when the risk of pulmonary embolism has subsided."
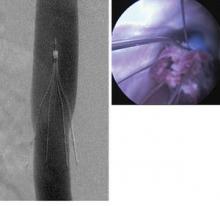
When Dr. Lazar Greenfield invented the filter in the early 1970s, it was intended to be used in patients at risk of a pulmonary embolism, but who had contraindications to anticoagulation therapy. Since that time, however, off-label use has expanded and filters proliferated. Now there are more than a dozen on the market, all approved by the FDA’s 510(k) process."In 2010, about 210,000 of these filters were deployed worldwide, but 85% of those were done in the U.S.," said Dr. Johnson, a professor of radiology and surgery at the Indiana University School of Medicine, Indianapolis, and a member of SIR. "In the best interest of our patients, this study will provide a systematic, functional view, repre- sentative of most filters placed in the United States. It will assist with quality improvement in filter placement, management, and retrieval."
There are no concrete answers because very little research has been done on the topic. A 2010 Cochrane review found just two IVC trials comprising 529 patients. One of those examined the filters’ use in hip fracture patients, but had just a 1-month follow-up period.
The other study – which experts call the only substantial look at the issue – was the 1998 PREPIC, which randomized 400 patients with DVT or PE to filter or no filter, with a total of 8 years’ follow-up.
"No reduction in mortality was seen," the Cochrane report noted, "but this reflected an older study population; the majority of deaths were due to cancer or cardiovascular causes." The filter group had an increased, though not significantly so, incidence of DVTs, and the trial didn’t report filter-associated adverse events. Because all patients in both arms of the trial received anticoagulation therapy, it’s possible that the benefits of the filters were diminished.
"PREPIC did IVC filters a huge disservice, because it said that filters didn’t provide any benefit but were associated with a trend toward increased risk," of clotting. Nor did the trial include most of the filters in use today, Dr. Johnson added, furthering limiting its usefulness.
Because of the paucity of data, the Cochrane review could not make a recommendation on filter use. PRESERVE is important because it will not only provide long-term safety and efficacy data for a broad range of filters, but also paint a picture of how they are used, and how patients who have them are cared for.
One of FDA’s biggest safety concerns was that filters designed to be retrievable are, essentially, becoming permanent, Dr. David Gillespie said in an interview. Dr. Gillespie, an SVS member and PRESERVE study director, believes the devices are over-used in the U.S., where "practically every trauma patient" receives one early in the course of treatment, when the risk of developing a clot is highest.