Low malignant potential tumors of the ovary: A review
Low malignant potential tumors of the ovary – otherwise known as borderline tumors – include ovarian tumors with atypical cellularity, which lack stromal invasion that differentiates them from low grade and high grade invasive carcinomas. They can coexist with extraovarian disease, however, in the setting of borderline tumors these foci are referred to as “implants” rather than metastases. As discussed below, these implants can exhibit the presence of invasion or not.
Classification
The two most common histologic categories of borderline tumors are serous and mucinous cell types. Rarer histologic types such as endometrioid, clear cell, and Brenner also exist. However, these are so infrequent that they will not be covered in this discussion as there are very limited data to make generalizations about these histologies.
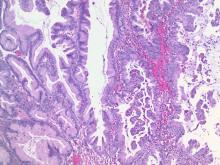
Serous borderline tumors contain cellularity similar to that of fallopian tubal epithelium. Approximately 25% of all serous ovarian tumors exhibit borderline features. Compared with mucinous tumors, they are more commonly bilateral and smaller in size (mean size of 12 cm) at the time of diagnosis and they are more likely to be associated with extraovarian implants (typically peritoneal). In fact, up to 25% of serous borderline tumors have concomitant extraovarian implants. Cancer antigen (CA) 125 is commonly a tumor marker for these tumors (elevated in 45% of early stage disease and 80% of advanced stage disease).1
Incidence
The incidence of borderline ovarian tumors is 2.5 per 100,000 woman years in the United States. About 70% are diagnosed at stage I.3 They arise in a younger population compared with invasive ovarian carcinomas. Risk factors for development of borderline tumors are similar to those of invasive ovarian carcinomas (such as nulliparity) but there may be a stronger association between the development of borderline ovarian tumors and infertility, as well as prior use of infertility treatment.4
Diagnosis
The diagnosis of borderline tumors of the ovaries occurs almost exclusively at the time of surgical pathology (either frozen section or definitive pathology).
Preoperative assessments with imaging and tumor markers – usually CA 125 and carcinoembryonic antigen (CEA) – are nonspecific for this tumor type. Preoperative imaging will typically reveal complex ovarian cysts with papillations and vascularity. However, in the case of mucinous borderline tumors, unilocular cysts are common.1 The presence of ascites and peritoneal implants can be observed on preoperative imaging of serous borderline tumors with extraovarian disease. However, it is not possible for this imaging to accurately differentiate borderline tumors with implants from low grade and high grade carcinomas with metastases.
Surgical management
Borderline tumors are commonly diagnosed in women of reproductive age and decisions need to be made regarding fertility sparing surgery, ovarian sparing surgery, and whether staging is performed. The recommended surgery for women who have completed child bearing is complete hysterectomy with bilateral salpingo-oophorectomy. However, cystectomy or unilateral salpingo-oophorectomy can be considered for women who desire fertility preservation. Conservative fertility preserving surgery is associated with an increased risk of recurrence, but with no negative impact on survival.1
Staging – with at least omentectomy and comprehensive evaluation of the peritoneal cavity, with or without peritoneal biopsies – can be considered, though staging is not associated with improved survival. Lymphadenectomy is also not associated with improved oncologic outcomes and routine lymphadenectomy is not recommended for borderline tumors.1 However, about a quarter of patients with gross evidence of extraovarian disease have implants within lymph nodes. Bulky lymph nodes should be removed, particularly in this group of patients.
Complete removal of extraovarian implants is the surgical intervention that is most important for survival and recurrence.1 This requires that surgeons thoroughly evaluate the peritoneal cavity and retroperitoneum, and possess the capability to completely resect all sites of disease.
Historically appendectomy was part of surgical staging of mucinous borderline tumors in order to identify a primary appendiceal lesion, but only 1% of patients with a grossly normal appearing appendix have significant pathology identified. This is no longer recommended.2