Impact of a Connected Care model on 30-day readmission rates from skilled nursing facilities
BACKGROUND
About one-fifth of hospitalized Medicare beneficiaries are discharged to skilled nursing facilities (SNFs) for post-acute care. Readmissions are common but interventions to reduce readmissions are scarce.
OBJECTIVE
To assess the impact of a connected care model on 30-day hospital readmission rates among patients discharged to SNFs.
DESIGN
Retrospective cohort.
SETTING
SNFs that receive referrals from an academic medical center in Cleveland, Ohio.
PARTICIPANTS
All patients admitted to Cleveland Clinic main campus between January 1, 2011 and December 31, 2014 and subsequently discharged to 7 intervention SNFs or 103 control SNFs.
INTERVENTION
Hospital-employed physicians and advanced practice professionals (nurse practitioners and physicianassistants) visited SNF patients 4 to 5 times per week.
RESULTS
During the study period, 13,544 patients were discharged to SNFs within a 25-miles radius of Cleveland Clinic main campus. Of these, 3334 were discharged to 7 intervention SNFs and 10,201 were discharged to 103 usual-care SNFs. During the intervention phase (2013-2014), adjusted 30-day readmission rates declined at the intervention SNFs (28.1% to 21.7%, P < 0.001), while there was a slight increase at control SNFs (27.1 % to 28.5%, P < 0.001). The absolute reductions ranged from 4.6% for patients at low risk for readmission to 9.1% for patients at high risk, and medical patients benefited more than surgical patients.
CONCLUSION
A program of frequent visits by hospital employed physicians and advanced practice professionals at SNFs can reduce 30-day readmission rates. Journal of Hospital Medicine 2017;12:238-244. © 2017 Society of Hospital Medicine
© 2017 Society of Hospital Medicine
Approximately 20% of hospitalized Medicare beneficiaries in the U.S. are discharged to skilled nursing facilities (SNFs) for post-acute care,1,2 and 23.5% of these patients are readmitted within 30 days.3 Because hospital readmissions are costly and associated with worse outcomes,4,5 30-day readmission rates are considered a quality indicator,6 and there are financial penalties for hospitals with higher than expected rates.7 As a result, hospitals invest substantial resources in programs to reduce readmissions.8-10 The SNFs represent an attractive target for readmission reduction efforts, since SNFs contribute a disproportionate share of readmissions.3,4 Because SNF patients are in a monitored environment with high medication adherence, risk factors for readmission likely differ between patients discharged to SNFs and those sent home. For example, 1 study showed that among heart failure patients with cognitive impairment, those discharged to SNFs had lower readmissions during the first 20 days, likely due to better medication adherence.11 Patients discharged to SNFs generally have more complex illnesses, lower functional status, and higher 1-year mortality than patients discharged to the community.12,13 Despite this, SNF patients might have infrequent contact with physicians. Federal regulations require only that patients discharged to SNFs need to be seen within 30 days and then at least once every 30 days thereafter.14 According to the 2014 Office of Inspector General report, one-third of Medicare beneficiaries in SNFs experience adverse events from substandard treatment, inadequate resident monitoring and failure or delay of necessary care, most of which are thought to be preventable.15
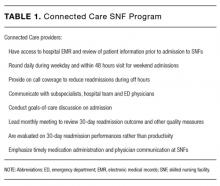
To address this issue, the Cleveland Clinic developed a program called “Connected Care SNF,” in which hospital-employed physicians and advanced practice professionals visit patients in selected SNFs 4 to 5 times per week, for the purpose of reducing preventable readmissions. The aim of this study was to assess whether the program reduced 30-day readmissions, and to identify which patients benefited most from the program.
METHODS
Setting and Intervention
The Cleveland Clinic main campus is a tertiary academic medical center with 1400 beds and approximately 50,000 admissions per year. In late 2012, the Cleveland Clinic implemented the Connected Care SNF program, wherein Cleveland Clinic physicians regularly visited patients who were discharged from the Cleveland Clinic main campus to 7 regional SNFs. Beginning in December 2012, these 7 high-volume referral SNFs that were not part of the Cleveland Clinic Health System (CCHS) agreed to participate in the program, which focused on reducing avoidable hospital readmissions and delivering quality care (Table 1). The Connected Care team, comprised of 2 geriatricians (1 of whom was also a palliative medicine specialist), 1 internist, 1 family physician, and 5 advanced practice professionals (nurse practitioners and physician assistants), provided medical services at the participating SNFs. These providers aimed to see patients 4 to 5 times per week, were available on site during working hours, and provided telephone coverage at nights and on weekends. All providers had access to hospital electronic medical records and could communicate with the discharging physician and with specialists familiar with the patient as needed. Prior to the admission, providers were informed about patient arrival and, at the time of admission to the SNF, providers reviewed medications and discussed goals of care with patients and their families. In the SNF, providers worked closely with staff members to deliver medications and timely treatment. They also met monthly with multidisciplinary teams for continuous quality improvement and to review outcomes. Patients at Connected Care SNFs who had their own physicians, including most long-stay and some short-stay residents, did not receive the Connected Care intervention. They constituted less than 10% of the patients discharged from Cleveland Clinic main campus.