“Hot tub” lung: Is it on your list of respiratory ailments?
A 49-year-old white male came to our Family Medicine Center with a complaint of lethargy, night sweats, fever, dyspnea on exertion, myalgias, and an 8-pound weight loss over a 4-week period. He was employed as a recreational director, and his normally athletic lifestyle had been limited by his symptomatic illness.
He had recently traveled to Mexico and Barbados and reported no known animal or insect bites. He had no history of lung disease or occupational exposure. He stopped smoking 5 years earlier (20-pack-year history) and did not use drugs. He had no infectious contacts or significant risk factors.
During the interview, he mentioned recently using an indoor hot tub ventilated with hose aeration. In fact, he used the hot tub almost daily for the 2 months leading up to this office visit. He developed symptoms after approximately 4 weeks of hot tub use.
What diagnostic studies showed
Baseline measurements were all within normal limits for a complete blood count, comprehensive metabolic panel, and thyroid-stimulating hormone. The sedimentation rate was elevated (76), as was C-reactive protein (62.3); an ANA with titer 1:80 showed homogenous pattern.
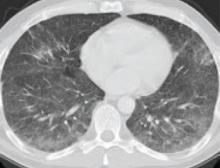
The chest x-ray was normal; however, a chest computed tomography (CT) scan performed 2 weeks after the initial film due to symptom exacerbation showed diffuse bilateral ground-glass opacification within the lung parenchyma (FIGURE 1). Pulmonary function testing revealed a mild to moderate restrictive defect with a decrease in the diffusion capacity.
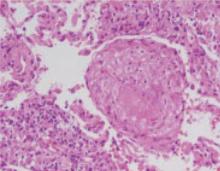
Transbronchial microscopic studies revealed noncaseating granulomatous inflammation (FIGURES 2 AND 3). Results were negative for acid-fast bacilli smears and for bacterial and fungal cultures from blood and bronchial washings.
FIGURE 1
CT scan of chest
Chest computed tomography scan showed groundglass opacification in lung parenchyma.
FIGURE 2
Microscopic evaluation of lung
Microscopic evaluation from bronchoscopy revealed noncaseating granulomatous inflammation consistent with hypersensitivity pneumonitis.
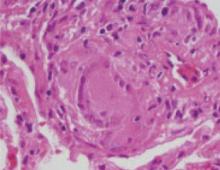
FIGURE 3
Lung granuloma
Image of an isolated lung granuloma from the microscopic evaluation in Figure 2.
Follow-up
This immunocompetent patient was diagnosed with interstitial hypersensitivity pneumonitis. A definitive organism was never isolated.
Hot tub pathogens
Hot tub lung is thought to be a hypersensitivity response to an aerosolized organism such as Mycobacterium avian complex (MAC), which is a common contaminant of standing water.1-4 (A point of controversy is whether persons with pulmonary disease secondary to nontuberculous mycobacterial disease are experiencing a hypersensitivity reaction to the organisms, or simply symptoms secondary to true pulmonary infection.5) Cladosporium spp and Bacillus cereus also can cause a hypersensitivity reaction.
More than one pathologic process?
For previously healthy patients who experience an abrupt onset of fever, chills, malaise, cough, chest tightness, and dyspnea, the differential diagnosis may be broad. However, a history of hot tub exposure makes a diagnosis of hypersensitivity pneumonitis likely. Infiltrates on CT scan,6 clinical improvement with avoidance of the allergen (with or without steroids), and absence of predisposing factors such as chronic lung disease are also consistent with hypersensitivity pneumonitis.
However, the noncaseating granulomatous inflammation found in our patient is suggestive of infection, and both MAC and Pseudomonas aeruginosa have been associated with poor hot tub maintenance.7 Some authors suggest that hot tub lung is a spectrum of disease with components of both hypersensitivity pneumonitis and infection.8-11
Treatment
The main focus of treatment is avoiding the allergen (the hot tub). Patients with persistent symptoms may benefit from a short course of oral corticosteroids. Antimycobacterial medications may be needed, depending on the symptoms and response to avoidance therapy.12 Antibacterials and antifungals are rarely needed.
After 4 weeks of steroid therapy and avoiding the hot tub, our patient was able to return to aerobic activity without symptoms. One year later, he had no long-term adverse effects.
Hot tub maintenance as disease prevention
Infections are more likely to occur if a hot tub is improperly maintained. Outbreaks of P aeruginosa dermatitis13 and otitis externa13 associated with hot tub use have been reported, as have the nonvenereal spread of herpes simplex virus from spa facilities.14 Severe necrotizing pneumonia due to community-acquired P aeruginosa was associated with a poorly maintained hot tub.8 Hot tub exposure during early pregnancy has been associated with an increased risk of neural tube defects.15
Hot tubs should be maintained according to manufacturer’s recommendations, which include both frequent water changes and adequate use of disinfectants. Proper usage also entails changing filters on schedule and showering before using a hot tub.
Water temperatures above 84°F may make chlorine evaporate and lose much of its disinfectant properties. Bromine is often substituted for chlorine because of its lower vapor pressure, but bromine is more reactive and may exacerbate the formation of antigens that may lead to a hypersensitivity reaction.