Cervical cancer screening: How our approach may change
Accumulating evidence has begun to alter priorities in testing modalities and in testing intervals, and further changes may be on the way.
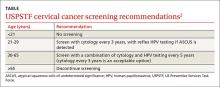
› Screen for cervical cancer in women ages 21 to 29 using cytology alone every 3 years. For women ages 30 to 65, screening with a combination of cytology and human papillomavirus (HPV) testing every 5 years is the preferred option. A
› Be aware of the alternative guideline proposed by several specialty organizations: All women ages 25 to 64 should receive primary HPV screening every 3 years with the FDA-approved HPV test. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
If the cervical cytology report you receive for a woman in her mid-20s is negative, how soon would you plan to repeat testing? Recommendations from the United States Preventive Services Task Force (USPSTF) and other leading organizations advise a combination of cytology and human papillomavirus (HPV) testing at specified intervals depending on a patient’s age. However, a study published in 2015 analyzed data from a statewide registry on provider behavior and found a wide array of screening intervals in practice and infrequent use of HPV testing.1 Clearly, adherence to published guidelines has been inconsistent.
Now, recommendations by several specialty groups are evolving based on newer evidence regarding HPV testing. These alternative guidelines recommend primary high-risk HPV testing for all women. This change is the topic of much national debate and is being researched for the USPSTF’s 2018 update on cervical cancer screening.
In this article, I review the USPSTF’s present recommendations and look ahead to how “best practices” for cervical cancer screening may be changing.
Current cervical cancer screening guidelines
Many subspecialty organizations and government agencies publish cervical cancer screening guidelines. The USPSTF guidelines, reviewed here, are evidence based, frequently updated, and widely used by primary care providers (TABLE).2,3 These guidelines recommend initiating cytology testing at age 21 and, if results are normal, repeating every 3 years. Reflex HPV testing is recommended if cytology results reveal atypical squamous cells of undetermined significance (ASCUS). For women ages 30 to 65, the preferred option is to undergo a combination of cytology and HPV testing every 5 years.2 Women older than 65 may discontinue screening.2 HPV immunization status does not affect USPSTF recommendations. Nationwide rates of HPV vaccination among females ages 13 to 17 vary among states, from ≤49% to ≥70%.4
What the guidelines do, and do not, cover. The USPSTF screening intervals apply as long as testing results are normal.2 These guidelines apply to all women regardless of the age at which they began sexual activity. These guidelines do not apply to women who have had abnormal cytology or HPV results and have not undergone adequate follow-up to ensure their lesion has cleared.5 These guidelines also do not apply to women who are immunosuppressed, who were exposed to diethylstilbestrol (DES) in utero, who have had a hysterectomy for non-oncologic reasons, or who have had cervical cancer.5 A woman may stop routine screening after age 65 if she has had adequate follow-up including either 3 negative cytology samples or 2 negative co-tests (cytology and HPV test) in the last 10 years.6 A woman may also discontinue screening if she has had a total hysterectomy and has no history of cervical dysplasia.7
Evidence behind the guidelines. The USPSTF guidelines were updated to their current state in 2012 reflecting a growing body of evidence that, for women 30 years and older, detection of cervical intraepithelial neoplasia (CIN) 3+ lesions improves with HPV co-testing. The supporting studies also found that the risk of a high-grade lesion appearing 5 years following co-testing was equivalent to the risk seen with cytology samples alone taken at 3-year intervals.8 The sensitivity of a single cytology test is only about 50%.9 A patient’s risk of cervical cancer 18 months after 3 negative cytology tests is about 1.5/100,000.10 The risk at 36 months following 3 negative cytology results is about 4.5/100,000. Annual screening would require almost 100,000 women to be screened to detect 3 additional cases of cervical cancer.10
Additional benefits of the updated USPSTF guidelines. The updated strategy decreases the number of visits for patients and the number of colposcopies, minimizing harm and patient anxiety. The current management algorithms also recommend more conservative management of women in their early 20s who have reported abnormal cytology, as the likelihood of their lesion clearing within 12 to 24 months is high.5 The recommendation does not call for high-risk HPV testing of women ages 21 to 29 because the infection is highly prevalent in this age group and is also likely to clear before any significant pathology arises. This avoids unnecessary and potentially harmful treatment of younger women.11