Kikuchi-Fujimoto Disease: A Case Report of Fever and Lymphadenopathy in a Young White Man
Background: Kikuchi-Fujimoto disease (KFD) is a rare cause of rapidly evolving tender cervical lymphadenopathy. It is often initially misdiagnosed and managed as infectious lymphadenitis. Although most cases of KFD are self-limited and improve with antipyretics and analgesics, some are more refractory and may require corticosteroids or hydroxychloroquine therapy.
Case Presentation: A 27-year-old White man presented for evaluation of fevers and painful cervical lymphadenopathy. He was found to have KFD on excisional lymph node biopsy. His symptoms proved challenging to manage with corticosteroids but eventually improved with hydroxychloroquine monotherapy.
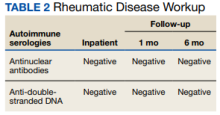
Conclusions: KFD diagnosis should be considered irrespective of geographic location, ethnicity, or patient sex. Hepatosplenomegaly is a relatively rare manifestation of KFD that can make it especially difficult to distinguish from lymphoproliferative disorder, such as lymphoma. Lymph node biopsy is the preferred diagnostic approach to achieve a timely and definitive diagnosis. Although usually self-limited, KFD has been associated with autoimmune conditions, including systemic lupus erythematosus. Securing the diagnosis of KFD is therefore crucial to ensuring patients are monitored appropriately for the development of associated autoimmune conditions.
Kikuchi-Fujimoto disease (KFD) is a rare, usually self-limited cause of cervical lymphadenitis that is more prevalent among patients of Asian descent.1 The pathogenesis of KFD remains unknown. Clinically, KFD may mimic malignant lymphoproliferative disorders, autoimmune diseases such as systemic lupus erythematosus (SLE) lymphadenitis, and infectious conditions such as HIV and tuberculous lymphadenitis. The most common presentation of KFD involves fever and rapidly evolving cervical lymphadenopathy.2,3 Due to its rarity, KFD is not always considered in the differential diagnosis for fever with tender lymphadenopathy, and up to one-third of cases are initially misdiagnosed.2
Definitive diagnosis requires lymph node biopsy. It is critical to achieving a timely diagnosis of KFD to exclude more serious conditions, initiate appropriate treatment, and minimize undue stress for patients. We describe a case of KFD in a patient who was met with delays in obtaining a definitive diagnosis for his symptoms.
Case Presentation
A 27-year-old previously healthy White man presented to the emergency department with subacute, progressive right-sided neck pain and swelling. In the week leading up to presentation, he also noted intermittent fevers, night sweats, and abdominal pain. His symptoms were unrelieved with acetaminophen and aspirin. He reported no sick contacts, recent travel, or animal exposures. He had no known history of autoimmune disease, malignancy, or immunocompromising conditions. Vital signs at the time of presentation were notable for a temperature of 39.0 °C. On examination, he had several firm, mobile, and exquisitely tender lymph nodes in the right upper anterior cervical chain. Abdominal examination was notable for left upper quadrant tenderness with palpable splenomegaly. Due to initial concern that his symptoms represented bacterial lymphadenitis, he was started on broad-spectrum antibiotics and admitted to the hospital for an expedited infectious workup.
Initial laboratory studies were notable for a white blood cell count of 3.7 × 109/L with 57.5% neutrophils and 27.0% lymphocytes on differential.