Multiple Cutaneous Abscesses Revealing Disseminated Nocardiosis in a Patient With Chronic Rheumatoid Arthritis
Nocardiosis is a challenging infection that is difficult to diagnose and treat. Delayed recognition and prolonged illness are major concerns. We report the case of a 65-year-old man who underwent treatment with corticosteroids for rheumatoid arthritis and then presented with multiple abscesses on the right leg. A complete assessment performed by the dermatologist led to the diagnosis of disseminated nocardiosis with involvement of the lungs and central nervous system. The patient’s history revealed development of pulmonary disease approximately 1 year prior to the appearance of the skin lesions, which was not recognized by several specialists. Long-term antibiotic therapy was effective in treating the skin and central nervous system lesions, while the chest radiologic profile improved more slowly.
- A high index of suspicion by the dermatologist is needed to alert the pathologist, microbiologist, and other clinicians involved in the assessment and diagnosis of nocardiosis.
- Because cultures from skin lesions of nocardiosis often show negative results, several specimens should be collected for analysis.
- Histopathologic analysis of skin biopsies often is necessary to exclude other inflammatory conditions and implicate an infectious process.
- Treatment with empirical broad-spectrum antibiotics should be promptly initiated and adjusted based on antibiotic susceptibility test results.
Nocardiosis is a rare human infection that has been reported worldwide but occurs more frequently in patients who reside in tropical areas. Although there is no predilection for age or ethnicity, nocardiosis is slightly more common in males than in females.1,2 The genus Nocardia belongs to the order Actinomycetales and includes more than 50 species of gram-positive, aerobic, filamentous, branching, partially acid-fast bacteria found ubiquitously in soil.3 The bacteria may be present in animals (eg, cattle, dogs),4 but transmission to humans is unusual. Clinical diagnosis of nocardiosis often is difficult because of its nonspecific manifestations and delays in its recognition, especially in western countries where the infection is consistently rare and probably underestimated.5-8 Cutaneous involvement generally manifests as 1 of 4 conditions: mycetoma, lymphocutaneous (sporotrichoid) infection, superficial skin infection, or systemic disease with cutaneous involvement.9 Systemic disseminated disease usually occurs in individuals with cellular immune deficiency, such as patients with human immunodeficiency virus; organ transplant recipients; or patients with a history of long-term use of corticosteroids, configuring an opportunistic infection.10-19 Incidence in these high-risk patients is 140- to 340-fold higher than in the general population.20Nocardia infections usually are acquired via dust inhalation, especially in dry environments. Focal pneumonitis is the first typical manifestation in immunosuppressed patients, followed by skin dissemination and central nervous system involvement.1
We report the case of a 65-year-old man who developed disseminated nocardiosis while undergoing long-term treatment with systemic corticosteroids for rheumatoid arthritis.
Case Report
A 65-year-old man presented to the dermatology department for evaluation of multiple papules and nodules with a puruloid discharge on the right leg. The first lesions had appeared on the right ankle approximately 1 month prior to presentation and were treated with systemic antibiotics by the patient’s general practitioner without remarkable benefits. The lesions progressed further on the right leg showing a sporotrichoid disposition.
On physical examination major involvement was evident on the right knee with papules, subcutaneous nodules, and sinuses (Figure 1). Isolated lesions also were present on the right thigh. A few days later some lesions were present on the left elbow and arm. Involvement of the popliteal and inguinal lymph nodes was noted, with painful enlarged nodules covered by erythematous skin that were mobile on deep planes. The lesions had a sudden onset while the patient was in good health, causing progressive functional impotency of the leg without general malaise or fever. The patient’s history was remarkable for chronic rheumatoid arthritis of 20 years’ duration that was treated with hydroxychloroquine (400 mg daily) and methylprednisolone (16 mg daily).
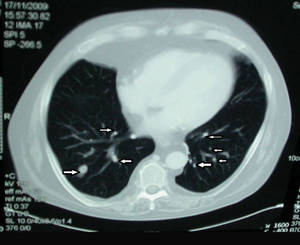
The patient was retired but reported daily tilling and manual labor on his farmland. He denied trauma or insect bites to the leg prior to the onset of lesions. Laboratory examination documented slight neutrophil leukocytosis (white blood cell count, 12.8×103/μL [reference range, 4.5–11.0×103/μL]; neutrophil count, 10.7×103/μL [reference range, 1.8–7.8×103/μL]; 85% neutrophils at formula count [reference range, 56%]), augmented C-reactive protein levels (15.8 mg/L [reference range, 0.08–3.1 mg/L]), a blood sedimentation rate of 74 mm/h (reference range, 0–20 mm/h), and elevated liver enzymes (aspartate aminotransferase, 52 U/L [reference range, 10–30 U/L]; alanine aminotransferase, 89 U/L [reference range, 10–40 U/L]; γ-glutamyltransferase, 68 U/L [reference range, 2–30 U/L]). Rheumatoid factor was 49.7 U/mL (reference range, 0–14.0 U/mL). Skin biopsy of a sample lesion suggested a chronic granulomatous suppuration. Tissue cultures and subsequent polymerase chain reaction assay identified Nocardia asteroides. A chest radiograph revealed multiple opaque nodules disseminated in both lungs, and a computed tomography (CT) scan confirmed multiple pulmonary lesions without involvement of the mediastinal lymph nodes (Figure 2). Computed tomography scans of the brain before and after contrast media perfusion showed the presence of an enhanced 8-mm mass among the right parietal and occipital lobes surrounded by an edematous halo (Figure 3). Neurologic examination was normal. During the radiologic assessment, the patient remembered having been hospitalized 1 year prior in a pulmonology unit at an outside institution for treatment of what was considered to be a multifocal nonspecific lung infection. A 1-month course of levofloxacin (500 mg daily) was administered at that time without any further follow-up. Review of the prior chest radiograph and CT scan confirmed the presence of the same radiologic findings as the current assessment, though of milder entity.
|

|







