Disruptive Physician Behavior: The Importance of Recognition and Intervention and Its Impact on Patient Safety
Professional misconduct by physicians is a significant problem with negative implications in the healthcare environment and has been termed "disruptive physician behavior" (DPB) in the United States. In recent years, hospitals and healthcare organizations have begun to better understand and formally address DPB, including its management and repercussions. Policy statements by the Joint Commission and the American Medical Association (AMA) have acknowledged that DPB may pose a threat to patient and provider safety. The purpose of this article is to raise awareness about the etiology of disruptive behavior in physicians, describe the consequences and the need for early recognition, and discuss potential interventions.
© 2018 Society of Hospital Medicine
Dramatic stories of disruptive physician behavior (DPB) appear occasionally in the news, such as the physician who shot and killed a colleague within hospital confines or the gynecologist who secretly took photographs using a camera disguised as a pen during pelvic examinations. More common in hospitals, however, are incidents of inappropriate behavior that may generate complaints from patients or other providers and at times snowball into administrative or legal challenges.
“Professionalism” is one of the six competencies listed by the Accreditation Council for Graduate Medical Education (ACGME)1 and the American Board of Medical Specialties. Unfortunately, incidents of disruptive behavior can result in violation of the tenets of professionalism in the healthcare environment. These behaviors fall along a continuum ranging from outwardly aggressive and uncivil to overly passive and insidious. Although these behaviors can occur across all healthcare disciplines and settings and are not just limited to physicians, the behaviors of physicians often have a much greater impact on the healthcare system as a whole because of their positions of relative “power” within the system.2 Hence, this problem requires greater awareness and education. In this context, the aim of this article is to discuss disruptive behaviors in physicians
The AMA defines DPB as “personal conduct, verbal or physical that has the potential to negatively affect patient care or the ability to work with other members of the healthcare team.”3 The definition of DPB by the Joint Commission includes “all behaviors that undermine a culture of safety.”4 Both the Joint Commission and the AMA recognize the significance and patient safety implications of such behavior. Policy statements by both these organizations underscore the importance of confronting and remedying these potentially dangerous interpersonal behaviors.
Data regarding the prevalence of DPB have been inconsistent. One study estimated that 3%–5% of physicians demonstrate this behavior,5 whereas another study reported a DPB prevalence of 97% among physicians and nurses in the workplace.6 According to a 2004 survey of physician executives, more than 95% of them reported regular encounters of DPB.7
The etiology of such disruptive behaviors is multifactorial and complex. Explanations associated with ‘nature versus nurture’ have ranged from physician psychopathology to unhealthy modeling during training. Both extrinsic and intrinsic factors may also contribute to DPB. External stressors and negative experiences–professional and/or personal–can provoke disruptive behaviors. Overwork, fatigue, strife, and a dysfunctional environment that can arise in both work and home environments can contribute to the development of mental health problems. Stress, burnout, and depression have increasingly become prevalent among physicians and can play a significant role in causing impaired patterns of professional conduct.8, 9 These mental health problems can cause physicians to acquire maladaptive coping strategies such as substance abuse and drug or alcohol dependence. However, it is important to note that physician impairment and substance abuse are not the most frequent causes of DPB. In fact, fewer than 10% of physician behavior issues have been related to substance abuse.2, 5
Psychiatric disorders such as major depression and bipolar and anxiety disorders may also contribute to DPB.10 Most of these disorders (except for schizophrenia) are likely as common among physicians as among the general public.9 An essential clarification is that although DPB can be a manifestation of personality disorders or psychiatric disorders, it does not always stem from underlying psychopathology. Clarifying these distinctions is important for managing the problem and calls for expert professional evaluation in some cases.10
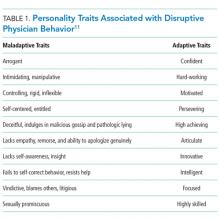
A person’s behavior is shaped by character, values, perceptions, and attitudes. Individuals who engage in DPB typically lack insight and justify their behaviors as a means to achieve a goal. Disrespectful behavior is rooted, in part, in characteristics such as insecurity, immaturity, and aggressiveness; however, it can also be learned, tolerated, and reinforced in the hierarchical hospital culture.11
Other intrinsic factors that may contribute to DPB include lack of emotional intelligence, poor social skills, cultural and ethnic issues, and generation and gender bias.12 Identifying the root causes of DPB can be challenging due to the complexity of the interaction between the healthcare environment and the key players within it; nevertheless, awareness of the contributing factors and early recognition are important. Those who take on the mantle of leadership within hospitals should be educated in this regard.