Cannabinoids and Digestive Disorders





Jami A. Kinnucan, MD, AGAF, FACG
Senior Associate Consultant
GI Practice Chair
Director of Digital Health and Practice Integration
Division of Gastroenterology and Hepatology
Department of Medicine
Mayo Clinic
Jacksonville, Florida
Disclosures:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Abbvie (Advisor, consultant); BMS (Advisor); Fresenius kabi (Advisor, consultant); Janssen (Advisor); Takeda (Advisor, consultant); Pfizer (Consultant)





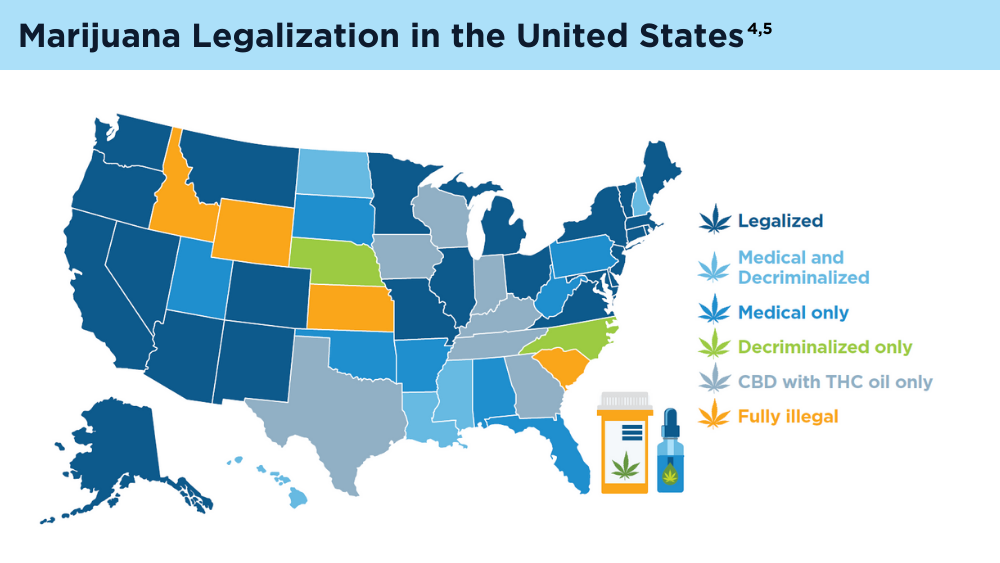
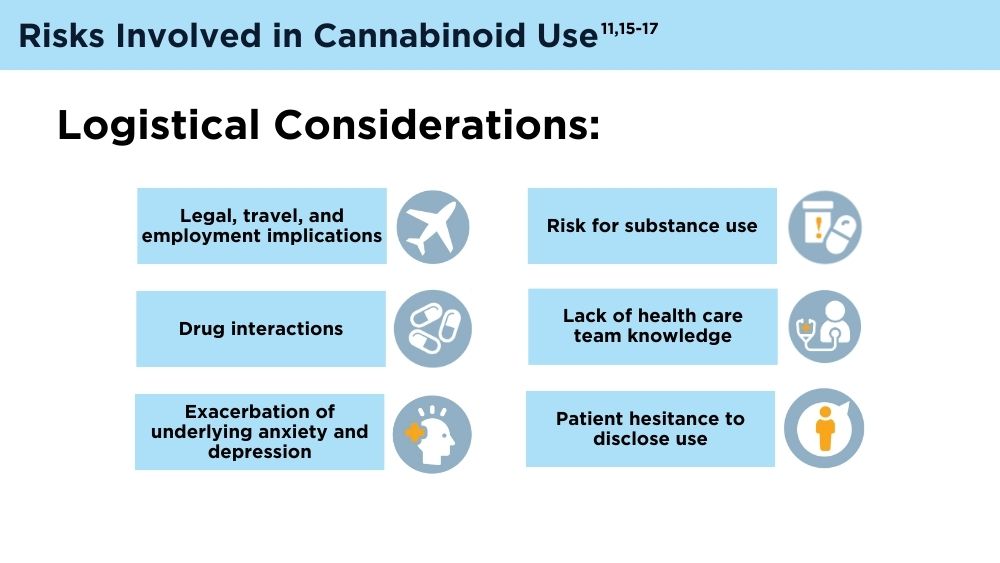
Complementary and alternative therapies are gaining interest in the gastrointestinal (GI) community. Up to 27% of adults in the United States and Canada report using cannabis for medical reasons, and up to 39% of patients with inflammatory bowel disease (IBD) report past use for symptom management.1-3 Significant questions and challenges still remain surrounding the use of cannabis in GI disorders, including its varied legalization status globally.4,5
Cannabinoids can be broken down into endocannabinoids (naturally occurring substances within the body) such as 2-arachidonoylgylcerol (2-AG) and anandamide (AEA), which act within the body at the cannabinoid receptors (CB) CB1 and CB2.6 There are also plant-based cannabinoids (phytocannabinoids) that include the most commonly known cannabidiol (CBD) and delta-9-tetrahydrocannabinol (THC). In addition, there are synthetic cannabinoids (manmade molecules that resemble THC or CBD), and synthetic receptor antagonists and agonists (manmade molecules that act directly at the cannabinoid receptors).
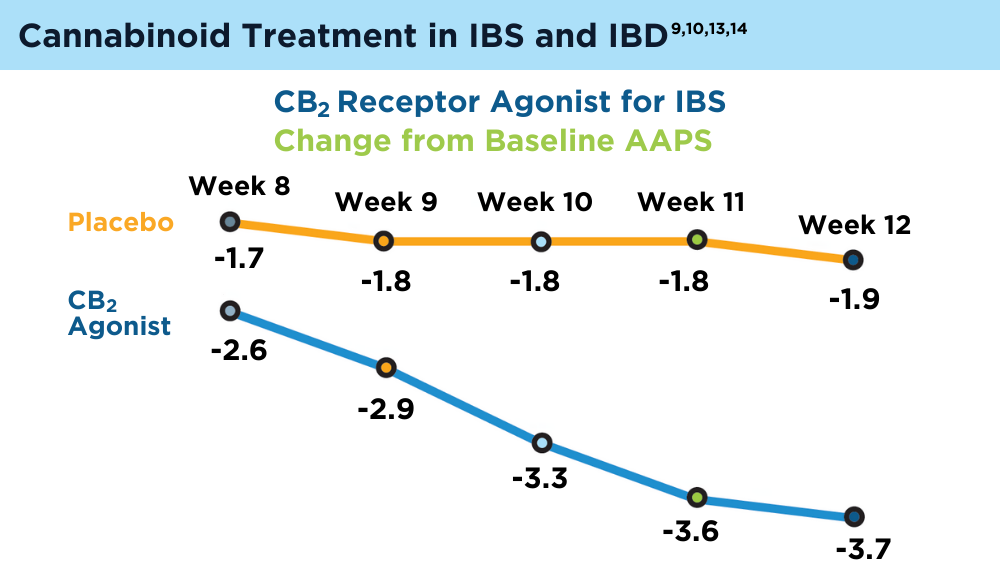
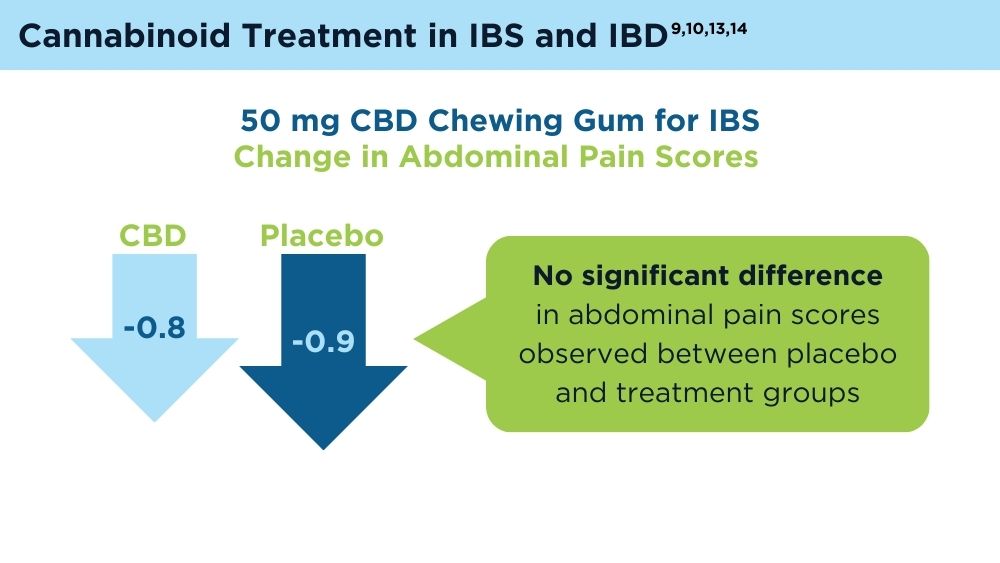
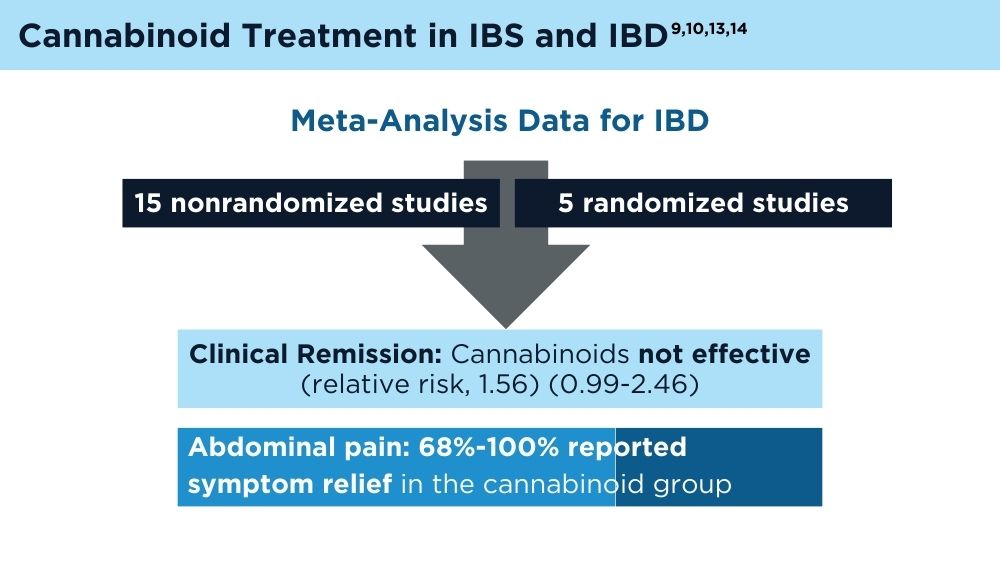
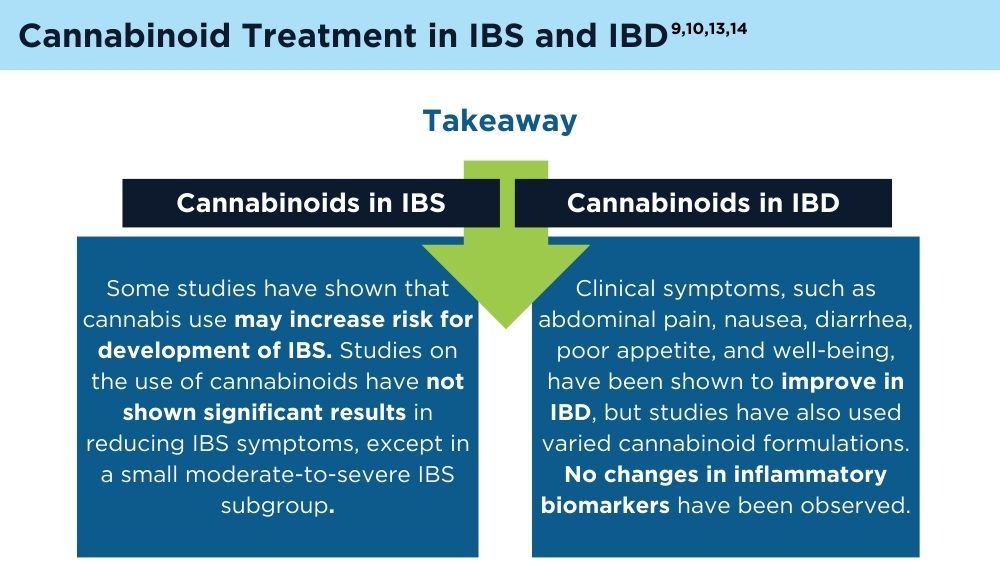
Studies have assessed cannabinoid use in many GI conditions—most notably IBD and irritable bowel syndrome (IBS)—however, medical marijuana use has only been approved in some states for Crohn’s disease or ulcerative colitis.4,7,8 In patients with IBS, there have been conflicting results, with a recent clinical trial of a synthetic CB2 agonist showing no significant change in abdominal pain scores.9 In patients with IBD, results are also varied, with some trials showing improvement in clinical measures but not endoscopic remission.10 These varied results could be due to differences in the formulation of cannabinoids studied and routes of administration.
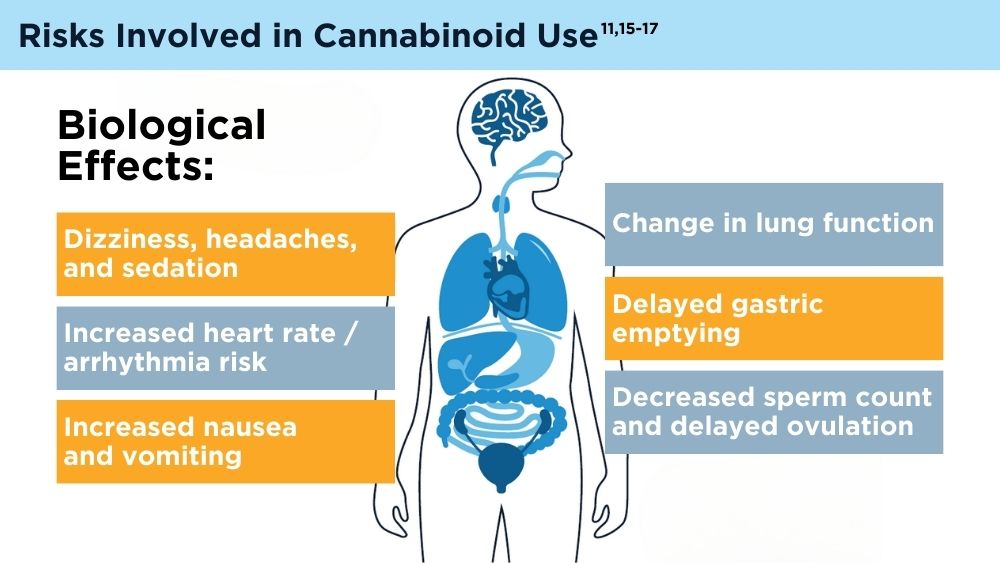
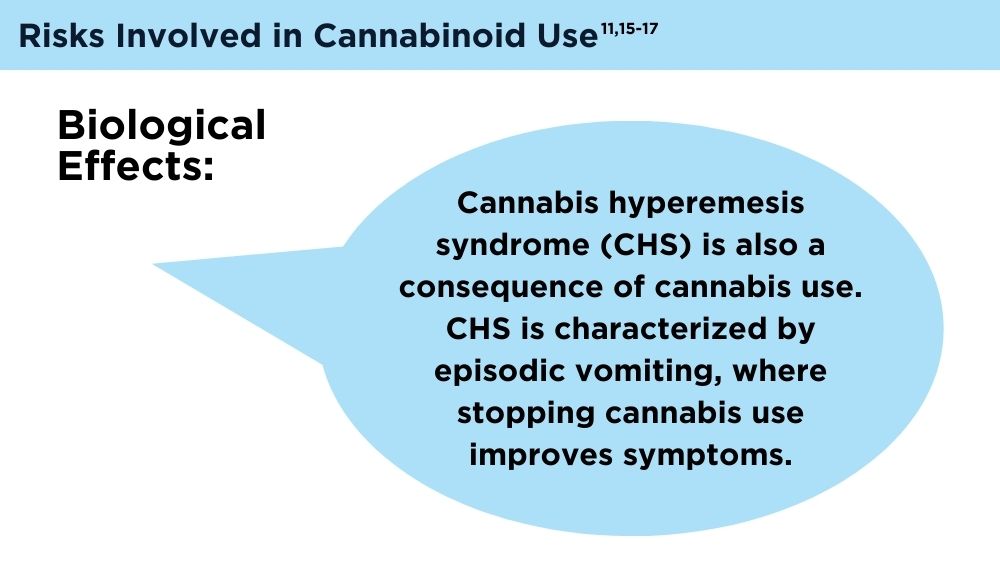
While the endocannabinoid system is of high interest within the GI community due to its therapeutic potential, many challenges remain, such as legalization, widely varied compounds and doses of active ingredients, and a lack of large, high-quality randomized studies.5,11,12 More research is needed to delineate the exact mechanism to best interact with the endocannabinoid system, and what GI disease states might be most affected.