The diagnosis
Answer to “What’s your diagnosis?” on page 2: Lemmel’s syndrome
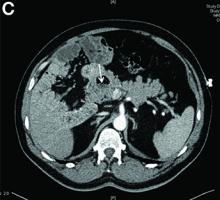
Figure C shows a 30 × 22-mm juxtapapillary diverticulum (JPD) containing air, fluid, and food debris (white arrow). Figure D shows the JPD (solid white arrow) causing distortion of a normal-caliber distal common bile duct (dashed white arrow) and pancreatic duct (PD; black arrow), with no gallbladder or ductal stones demonstrated. The final diagnosis was cholangitis and pancreatitis associated with a JPD without choledocholithiasis (Lemmel’s syndrome). He remains well 2 months later on follow-up, with normal blood tests.
Duodenal diverticuli occur commonly (15%–20% of autopsies), especially in the elderly, are usually discovered incidentally, and mostly asymptomatic. The majority (75%) are periampullary; those located within 2–3 cm of the ampulla of Vater are called JPD. Patients may rarely present with symptoms including abdominal pain, steatorrhea, gastrointestinal bleeding, perforation, intestinal obstruction, diverticulitis, and cholangiopancreatic disease (obstructive jaundice, cholangitis, and pancreatitis).1 Primary choledocholithiasis occurs commonly (incidence 20%–40%) in patients with periampullary duodenal diverticuli, owing to the production of beta-glucuronidase producing microorganisms. However, many patients (up to 41%) with JPD and cholangiopancreatic symptoms have normal biliary and pancreatic ducts on cholangiography.1,2 Lemmel’s syndrome is the combination of JPD and cholangiopancreatic disease without choledocholithiasis.3 It is postulated to arise from the reflux of duodenal contents with intestinal bacteria into the common bile duct and pancreatic duct, mechanical compression, or distortion of the distal common bile duct and pancreatic duct arising from an impacted enterolith or food debris in the diverticulum, or sphincter of Oddi dysfunction, with resultant bile stasis.1 Patients characteristically describe postprandial epigastric pain or fullness. The mainstay of treatment in the majority of patients is conservative, although endoscopic removal of impacted food debris may occasionally be necessary. Operative intervention, preferably duodenojejunostomy, may be indicated for persistent/recurrent symptoms or severe complications (such as recurrent cholangitis/pancreatitis, bleeding or perforation).
References
1. Egawa, N., Anjiki, H., Takuma, K., et al. Juxtapapillary duodenal diverticula and pancreatobiliary disease. Dig Surg. 2010;27:105-9.
2. Lobo, D.N., Balfour, T.W., Iftikhar, S.Y. Periampullary diverticula: consequences of failed ERCP. Ann Royal Coll Surg. 1998;80:326-31.
3. Lemmel, G. Die klinische Bedeutung der Duodenaldivertikel. Archiv fur Verdauungskrankheiten. 1934;56:59-70.