Breast and Uterine Cancer: Screening Guidelines, Genetic Testing, and Mortality Trends





Haley A. Moss, MD, MBA
Assistant Professor, Department of
Obstetrics and Gynecology
Duke University;
Director, Department of Veterans Affairs
Breast and Gynecologic Oncology System
of Excellence
Durham, North Carolina
Dr. Moss has no relevant financial relationships to disclose.





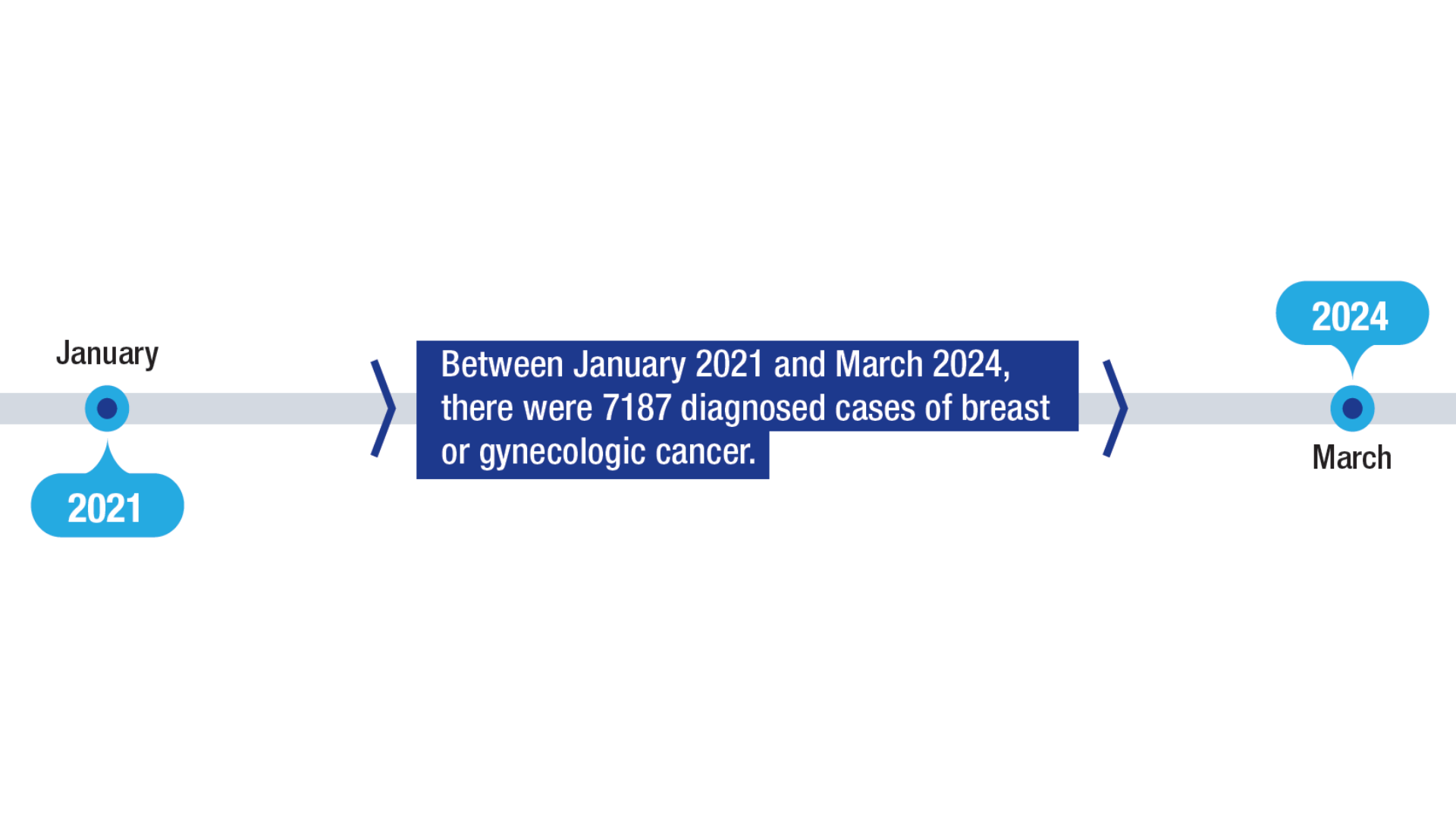
The VHA Breast and Gynecologic Oncology System of Excellence (BGSoE), established in 2021, provides comprehensive, high-quality cancer care tailored to veterans diagnosed with breast and gynecologic cancers and those considered high-risk based on genetic testing or family history.1 Since its inception, the BGSoE has supported more than 7000 patients.1 For breast cancer, new USPSTF guidelines now recommend initiating biennial mammography at age 40, reflecting efforts to address rising incidence in younger populations.2 The VHA recommends genetic testing for all veterans diagnosed with invasive breast cancer in order to expand access to targeted therapies, facilitate risk reduction for secondary cancers, and enable cascade testing for at-risk family members.3,4
Uterine cancer is a growing concern for veterans, with rising incidence and mortality, particularly in aggressive nonendometrioid subtypes.5,6 Black women in particular have higher uterine cancer mortality rates. This is of particular relevance within the VA, as Black women are overrepresented compared to the general population.6,7 This disparity underscores the need to improve outcomes for all patients while prioritizing targeted interventions for Black women.
 Women Veterans Treated Through the BGSoE1
Women Veterans Treated Through the BGSoE1
Within the veteran population, women are the fastest-growing group and face considerable risk factors for cancer. The VHA established the BGSoE to provide teleoncology and other cancer navigation services to women veterans.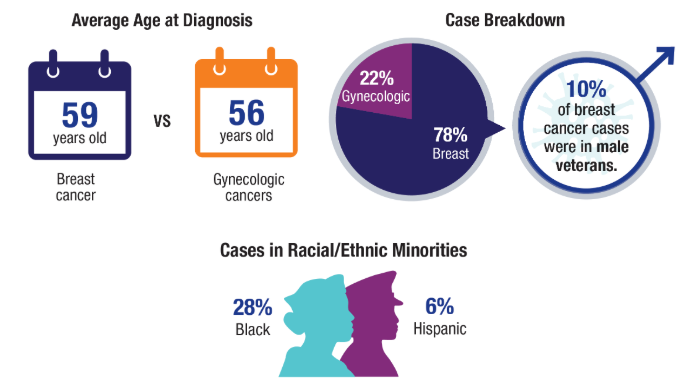 Women Veterans Treated Through the BGSoE1
Women Veterans Treated Through the BGSoE1
The VA is ensuring review of these programs through the Center for Oncology Outcomes Review and Gender (COURAGE).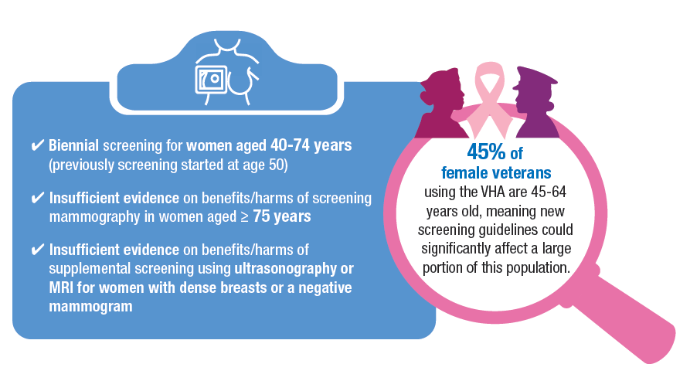 Updated 2024 Breast Cancer Screening Guidelines2,8
Updated 2024 Breast Cancer Screening Guidelines2,8
Breast cancer incidence is increasing among younger women, with a 2.0% average annual increase in incidence from 2015 to 2019 in women aged 40 to 49 years. In response, the USPSTF updated its guidelines to start screening as early as age 40.2 Other breast cancer screening guidelines, such as those for the National Comprehensive Cancer Network (NCCN) and the American Cancer Society (ACS), have also lowered the screening age for average risk to age 40.9,10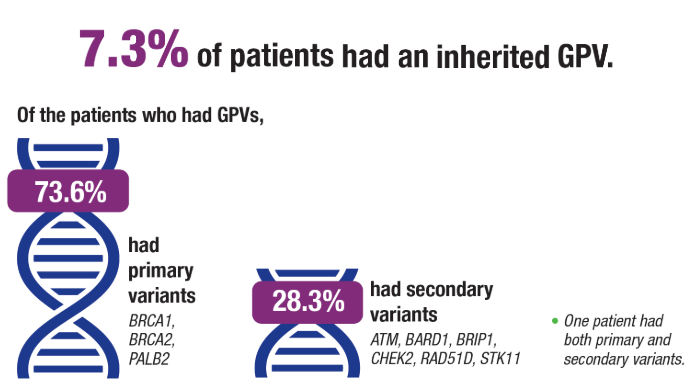 Universal Genetic Testing in Breast Cancer4
Universal Genetic Testing in Breast Cancer4
Traditional genetic testing criteria misses a portion of cases that could benefit from targeted therapies such as polyadenosine diphosphate polymerase (PARP) inhibitors, with 5-10% of breast cancer cases associated with germline pathogenic variants (GPVs). As genetic testing costs decrease and more treatments become available, there has been a push for universal genetic testing to help identify additional patients who may have otherwise been considered ineligible for targeted therapies. A recent study sought to evaluate the prevalence of GPVs in an ethnically diverse cohort of women with newly diagnosed invasive breast cancer.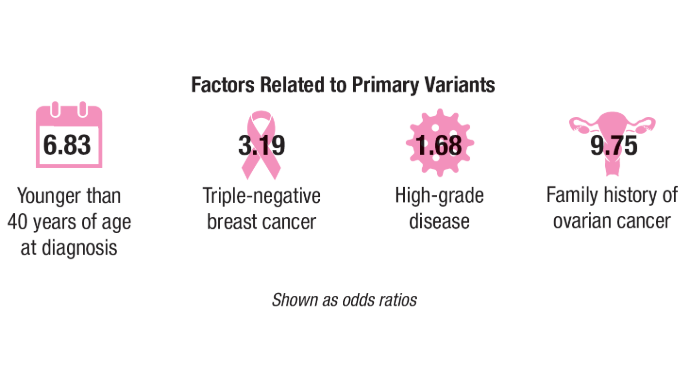 Universal Genetic Testing in Breast Cancer4
Universal Genetic Testing in Breast Cancer4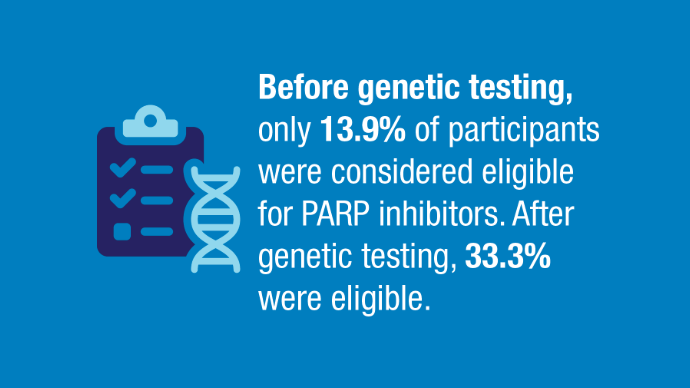 Universal Genetic Testing in Breast Cancer4
Universal Genetic Testing in Breast Cancer4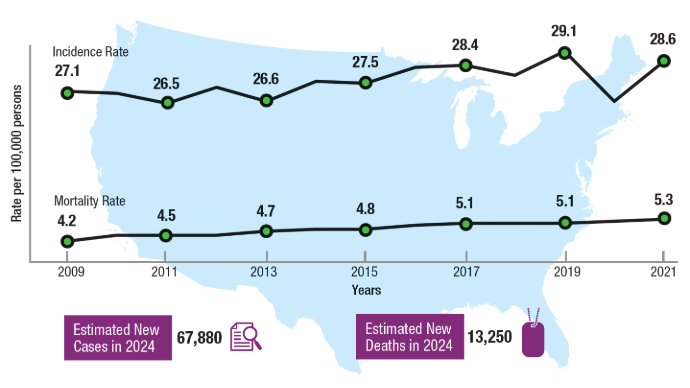 Uterine Cancer US Incidence and Mortality Rates5
Uterine Cancer US Incidence and Mortality Rates5
In most cancers, coinciding with increasing incidence, mortality tends to decrease, owing to the availability of new treatments. Uterine cancer is one of the few cancers with both rising incidence and mortality and without a clear cause or specific factor to address.5 The average annual percent increase in uterine cancer mortality is highest in women aged 49 years and younger.11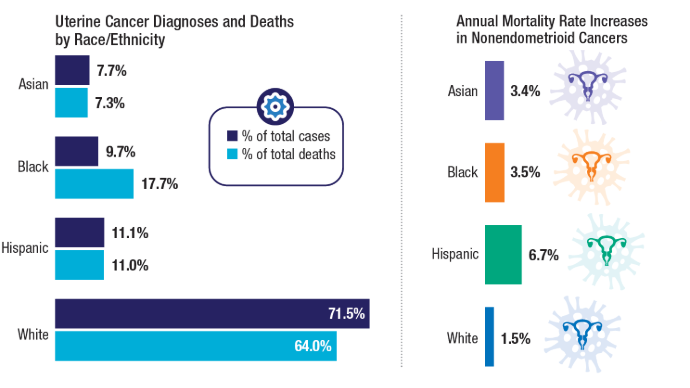 US Racial/Ethnic Uterine Cancer Trends6
US Racial/Ethnic Uterine Cancer Trends6
Racial disparities in uterine cancer are evident across incidence, subtypes, and mortality. Incidence of aggressive nonendometrioid subtypes, which disproportionately affect Black women, is increasing. Uterine cancer mortality rates are also higher among Black women, who account for < 10% of incident uterine cancer cases but nearly 18% of the total deaths from the disease.6 Within in the VA, Black women also comprise a higher percentage of uterine cancer cases.7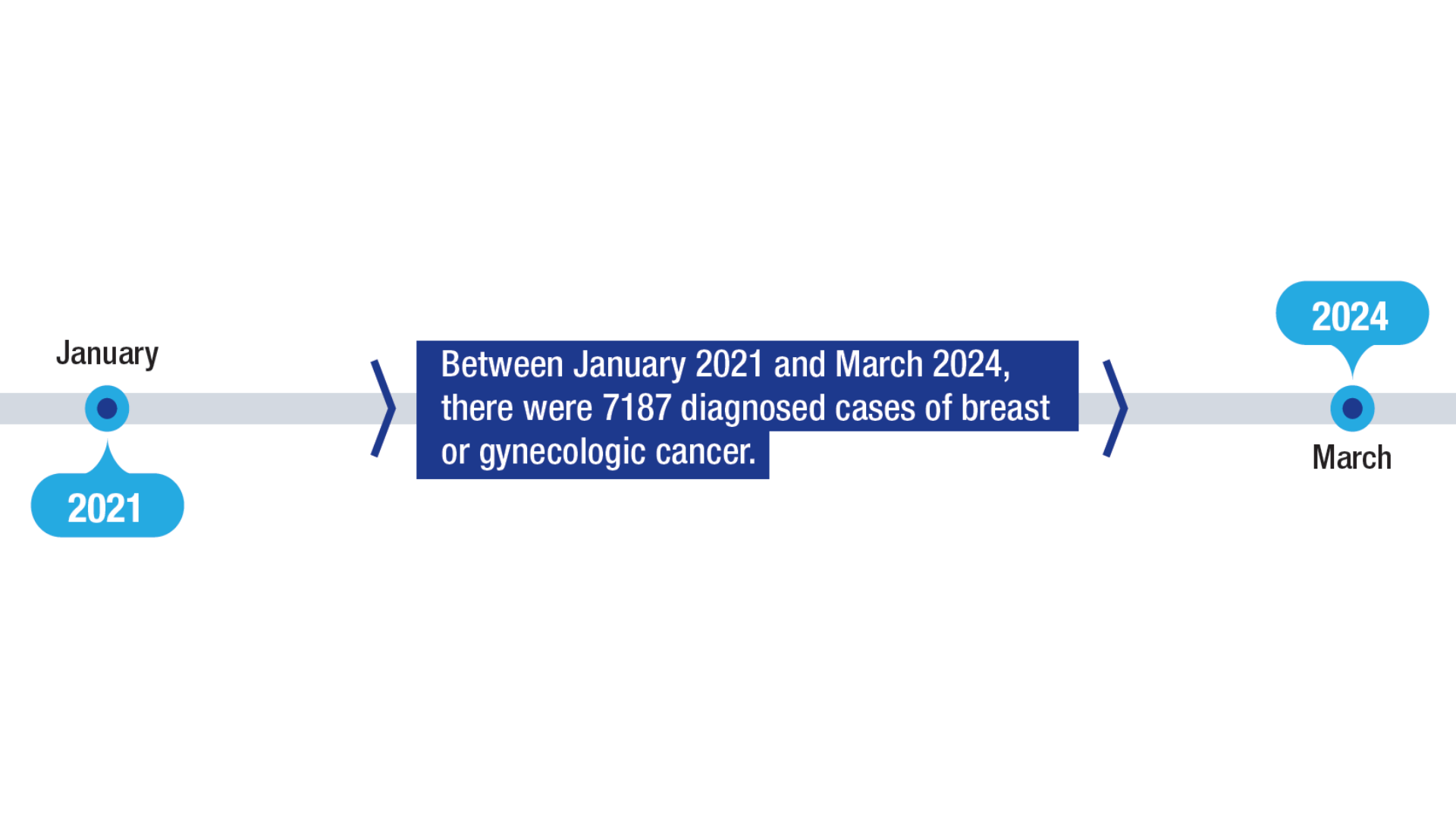 Women Veterans Treated Through the BGSoE1
Women Veterans Treated Through the BGSoE1
Within the veteran population, women are the fastest-growing group and face considerable risk factors for cancer. The VHA established the BGSoE to provide teleoncology and other cancer navigation services to women veterans.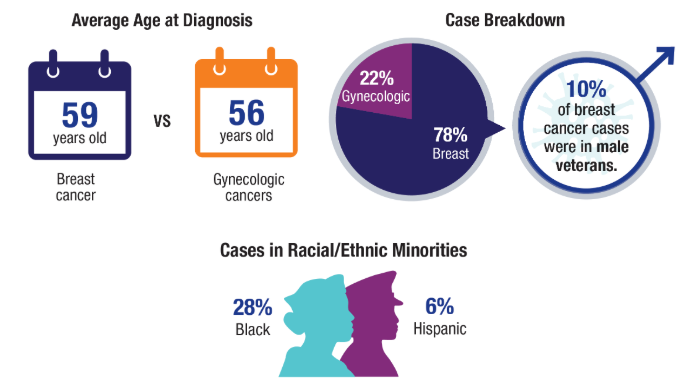 Women Veterans Treated Through the BGSoE1
Women Veterans Treated Through the BGSoE1
The VA is ensuring review of these programs through the Center for Oncology Outcomes Review and Gender (COURAGE).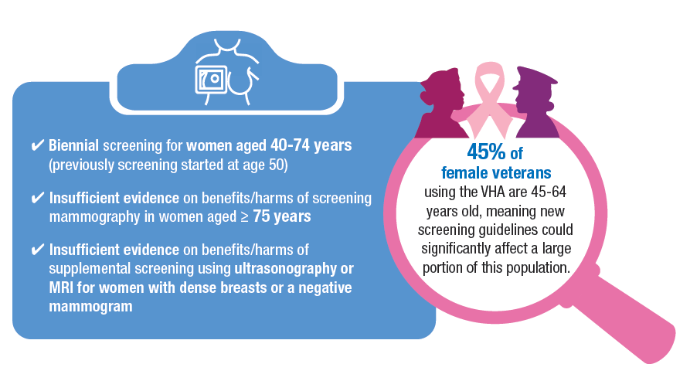 Updated 2024 Breast Cancer Screening Guidelines2,8
Updated 2024 Breast Cancer Screening Guidelines2,8
Breast cancer incidence is increasing among younger women, with a 2.0% average annual increase in incidence from 2015 to 2019 in women aged 40 to 49 years. In response, the USPSTF updated its guidelines to start screening as early as age 40.2 Other breast cancer screening guidelines, such as those for the National Comprehensive Cancer Network (NCCN) and the American Cancer Society (ACS), have also lowered the screening age for average risk to age 40.9,10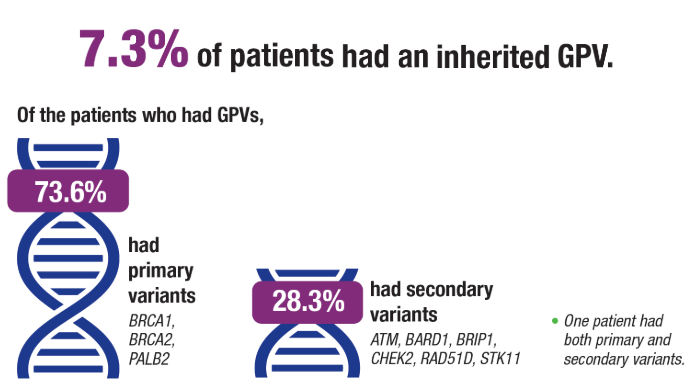 Universal Genetic Testing in Breast Cancer4
Universal Genetic Testing in Breast Cancer4
Traditional genetic testing criteria misses a portion of cases that could benefit from targeted therapies such as polyadenosine diphosphate polymerase (PARP) inhibitors, with 5-10% of breast cancer cases associated with germline pathogenic variants (GPVs). As genetic testing costs decrease and more treatments become available, there has been a push for universal genetic testing to help identify additional patients who may have otherwise been considered ineligible for targeted therapies. A recent study sought to evaluate the prevalence of GPVs in an ethnically diverse cohort of women with newly diagnosed invasive breast cancer.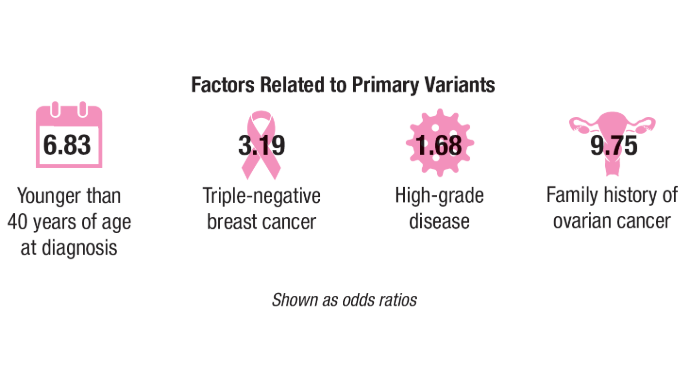 Universal Genetic Testing in Breast Cancer4
Universal Genetic Testing in Breast Cancer4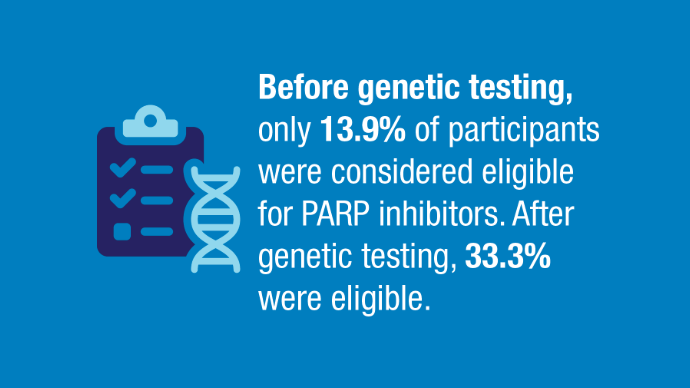 Universal Genetic Testing in Breast Cancer4
Universal Genetic Testing in Breast Cancer4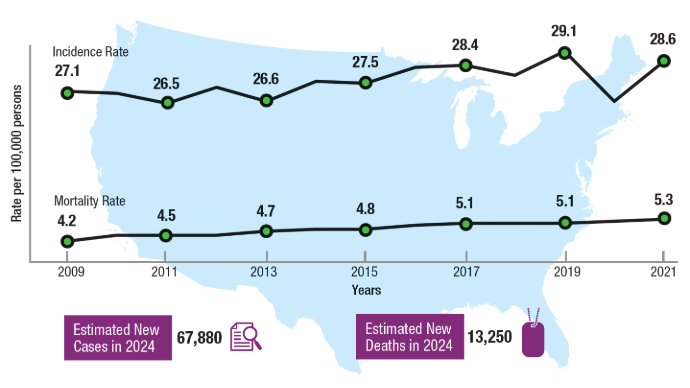 Uterine Cancer US Incidence and Mortality Rates5
Uterine Cancer US Incidence and Mortality Rates5
In most cancers, coinciding with increasing incidence, mortality tends to decrease, owing to the availability of new treatments. Uterine cancer is one of the few cancers with both rising incidence and mortality and without a clear cause or specific factor to address.5 The average annual percent increase in uterine cancer mortality is highest in women aged 49 years and younger.11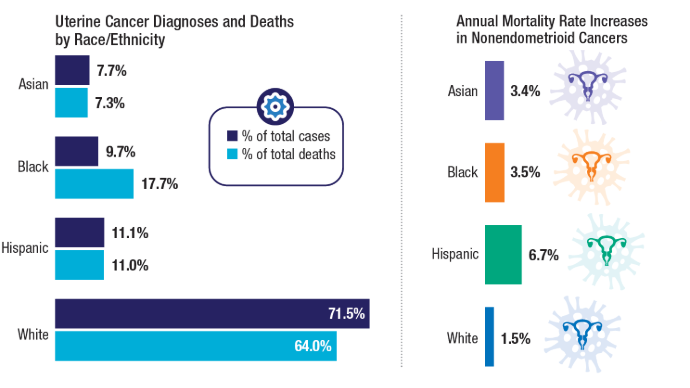 US Racial/Ethnic Uterine Cancer Trends6
US Racial/Ethnic Uterine Cancer Trends6
Racial disparities in uterine cancer are evident across incidence, subtypes, and mortality. Incidence of aggressive nonendometrioid subtypes, which disproportionately affect Black women, is increasing. Uterine cancer mortality rates are also higher among Black women, who account for < 10% of incident uterine cancer cases but nearly 18% of the total deaths from the disease.6 Within in the VA, Black women also comprise a higher percentage of uterine cancer cases.7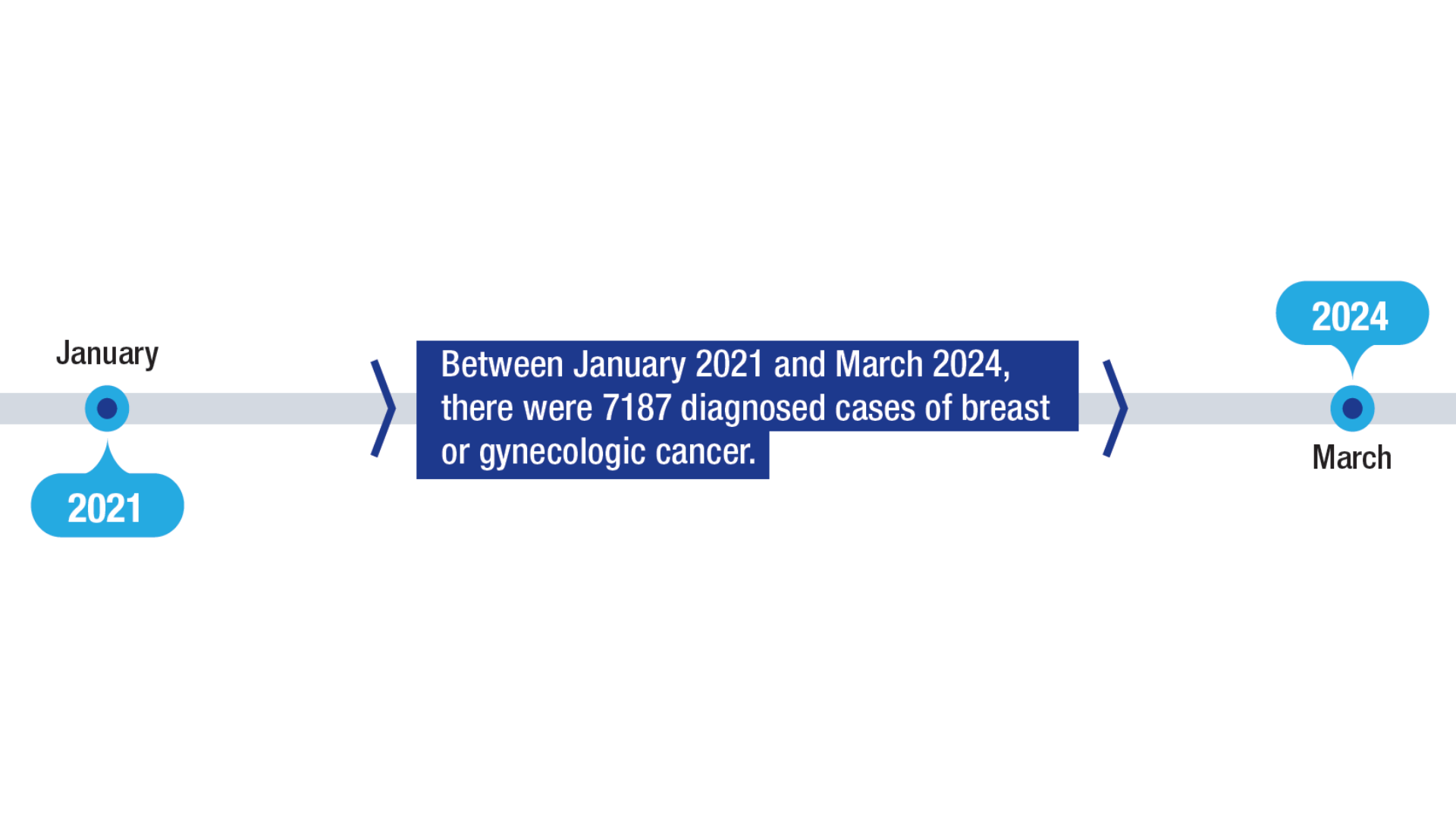 Women Veterans Treated Through the BGSoE1
Women Veterans Treated Through the BGSoE1
Within the veteran population, women are the fastest-growing group and face considerable risk factors for cancer. The VHA established the BGSoE to provide teleoncology and other cancer navigation services to women veterans.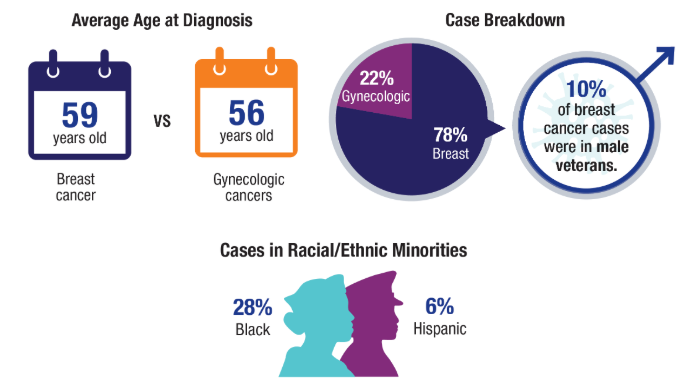 Women Veterans Treated Through the BGSoE1
Women Veterans Treated Through the BGSoE1
The VA is ensuring review of these programs through the Center for Oncology Outcomes Review and Gender (COURAGE).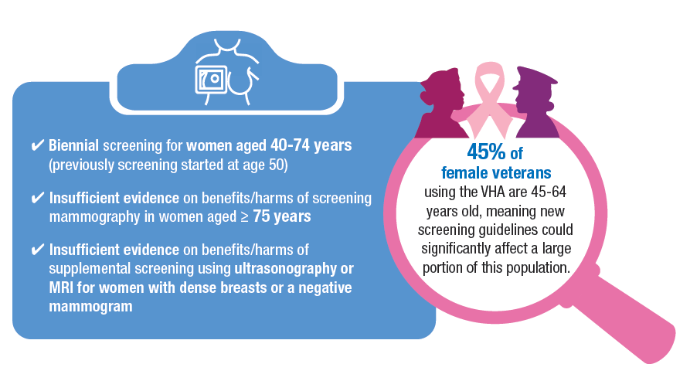 Updated 2024 Breast Cancer Screening Guidelines2,8
Updated 2024 Breast Cancer Screening Guidelines2,8
Breast cancer incidence is increasing among younger women, with a 2.0% average annual increase in incidence from 2015 to 2019 in women aged 40 to 49 years. In response, the USPSTF updated its guidelines to start screening as early as age 40.2 Other breast cancer screening guidelines, such as those for the National Comprehensive Cancer Network (NCCN) and the American Cancer Society (ACS), have also lowered the screening age for average risk to age 40.9,10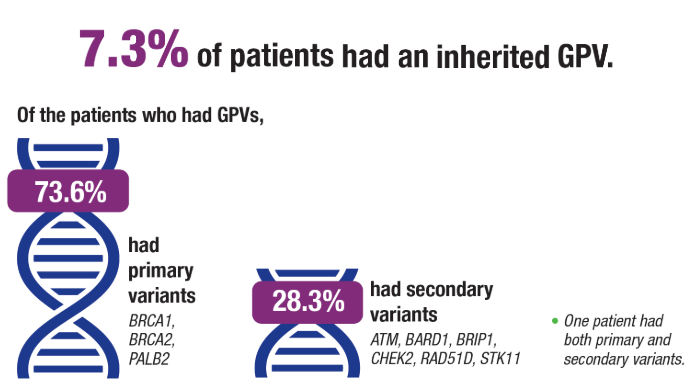 Universal Genetic Testing in Breast Cancer4
Universal Genetic Testing in Breast Cancer4
Traditional genetic testing criteria misses a portion of cases that could benefit from targeted therapies such as polyadenosine diphosphate polymerase (PARP) inhibitors, with 5-10% of breast cancer cases associated with germline pathogenic variants (GPVs). As genetic testing costs decrease and more treatments become available, there has been a push for universal genetic testing to help identify additional patients who may have otherwise been considered ineligible for targeted therapies. A recent study sought to evaluate the prevalence of GPVs in an ethnically diverse cohort of women with newly diagnosed invasive breast cancer.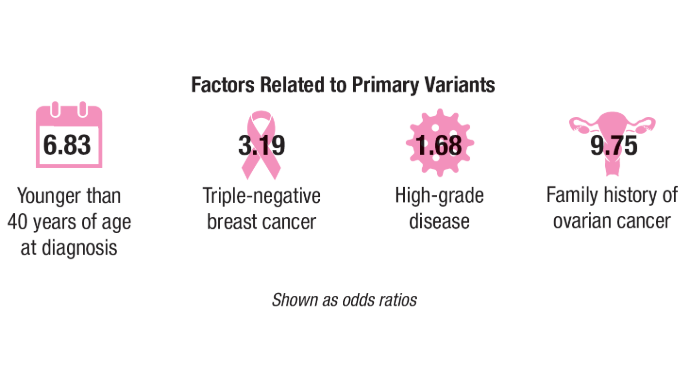 Universal Genetic Testing in Breast Cancer4
Universal Genetic Testing in Breast Cancer4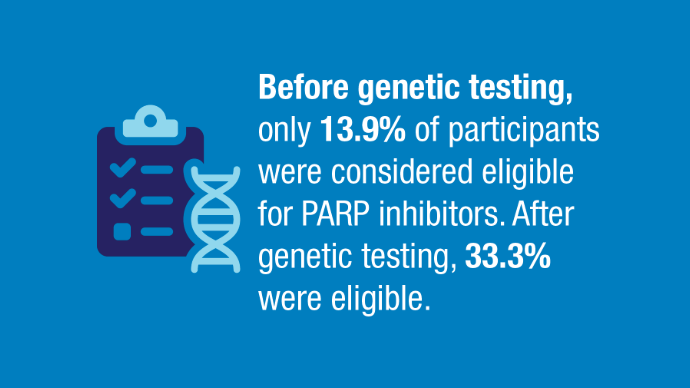 Universal Genetic Testing in Breast Cancer4
Universal Genetic Testing in Breast Cancer4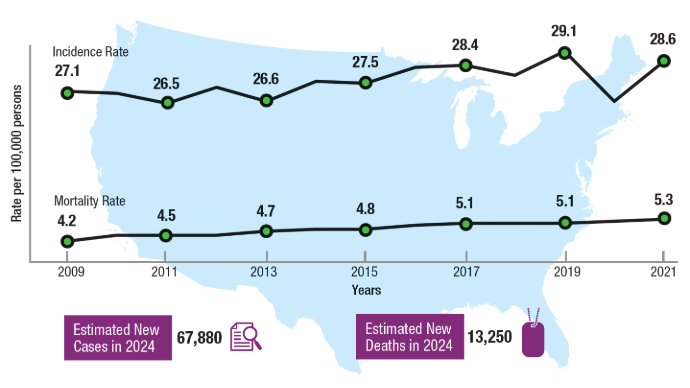 Uterine Cancer US Incidence and Mortality Rates5
Uterine Cancer US Incidence and Mortality Rates5
In most cancers, coinciding with increasing incidence, mortality tends to decrease, owing to the availability of new treatments. Uterine cancer is one of the few cancers with both rising incidence and mortality and without a clear cause or specific factor to address.5 The average annual percent increase in uterine cancer mortality is highest in women aged 49 years and younger.11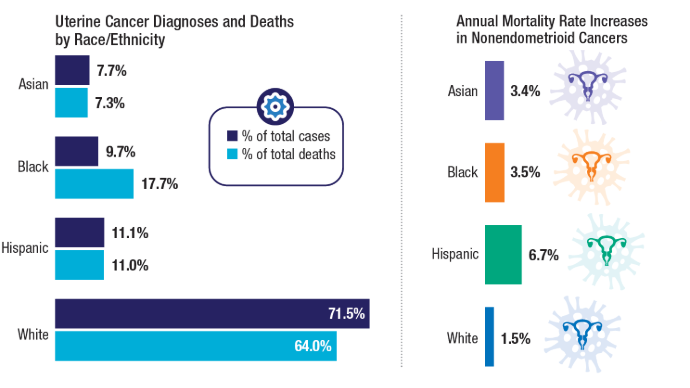 US Racial/Ethnic Uterine Cancer Trends6
US Racial/Ethnic Uterine Cancer Trends6
Racial disparities in uterine cancer are evident across incidence, subtypes, and mortality. Incidence of aggressive nonendometrioid subtypes, which disproportionately affect Black women, is increasing. Uterine cancer mortality rates are also higher among Black women, who account for < 10% of incident uterine cancer cases but nearly 18% of the total deaths from the disease.6 Within in the VA, Black women also comprise a higher percentage of uterine cancer cases.7
Click to view more from Cancer Data Trends 2025.
,false