Paclitaxel-eluting stent approved for PAD
The Food and Drug Administration has approved a new paclitaxel-eluting stent indciated for the treatment of peripheral artery disease.
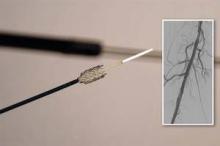
The Zilver PTX Drug-Eluting Peripheral Stent, which is manufactured by Cook Medical of Bloomington, Ind., is the first drug-eluting stent to win approval for this indication.
The approval was based on findings from both a randomized controlled trial and on a registry study, which together comprised more than 1,200 patients.
According to an FDA press statement, the studies indicate that treatment with the stent "is at least as safe as treatment with percutaneous transluminal angioplasty (PTA) and significantly more effective."
The randomized trial included a total of 479 patients who had a single stenotic lesion less than 140 mm in one or both of the femoropopliteal arteries.
The patients were randomized to the paclitaxel-eluting stent or to PTA. If the transluminal procedure failed, then the patients received either the paclitaxel-eluting stent or a bare-metal stent.
After 12 months, 83% of the arteries treated with the drug-eluting stent were still open, compared with 33% of those in the PTA group.
In those patients who had the stent placed after a failed PTA, 90% of arteries were open, compared with 73% in those who got the bare-metal stent.
In October 2011, the FDA's Circulatory System Devices Panel voted 11 to 0 that the benefits of the Zilver PTX stent outweighed its risks as a treatment for patients with symptomatic atherosclerotic stenosis of the femoropopliteal arteries on the basis of that trial.
This past October, the 3-year results of the study were presented at the Vascular Interventional Advances 2012 meeting in Las Vegas. The results showed that there was a 70.7% primary patency seen for the paclitaxel-eluting stent, compared with 49.1% for PTA and bare-metal stents.
The registry study followed 767 patients for 24 months. These patients had a maximum of four stents placed; the stents could be utilized to treat a single lesion or to treat multiple lesions.
At 12 months, the fracture rate was 1.5%; fractures were not associated with any clinical problems. The rate of stent thrombosis was 2.8% at 12 months and 3.5% at 24 months.
"The clinical study demonstrated that the [the paclitaxel-eluting stent] is more effective than the use of balloon angioplasty for the treatment of symptomatic peripheral artery disease in above-the-knee femoropopliteal artery," Christy Foreman, director of the Office of Device Evaluation at the FDA's Center for Devices and Radiological Health, said in the statement.
"This approval expands the treatment options for patients suffering from symptomatic peripheral artery disease," she added.
In both studies, the most common major adverse event was restenosis requiring additional treatment to reestablish adequate flow in the artery.
The device is contraindicated in patients with stenoses that cannot be dilated to permit passage of the catheter or proper placement of the stent.
It is also contraindicated in patients who cannot receive recommended drug therapy due to bleeding disorders, or women who are pregnant, breastfeeding, or planning to become pregnant in the next 5 years.
The FDA will now require the manufacturer to conduct a 5-year postapproval study of 900 patients to further evaluate the stent's safety and efficacy.