Data Trends 2025: Hepatology





Reviewed by:
Basile Njei, MD, PhD, MPH, Fulbright Professor of Global Health, Yale University; Associate Director, Yale Liver Center, New Haven, Connecticut. Basile Njei, MD, PhD, MPH, has disclosed no relevant financial relationships.





Screening rates in veterans are low for a variety of hepatologic diseases, such as metabolic dysfunction-associated steatotic liver disease (MASLD), hepatitis C virus (HCV), and hepatitis B virus (HBV).1,2 The veteran population has a high prevalence of metabolic and cardiovascular comorbidities, which are risk factors for MASLD.1,3 Veterans receiving VHA care also have a higher prevalence of HCV compared to the general US population.4 The VHA has achieved high HCV treatment and sustained virologic response (SVR) rates due to widespread use of direct-acting antivirals (DAAs).4 Within 5 years of diagnosis, about 2.5% of patients with MASLD progress to cirrhosis, with higher rates observed in certain races and ethnicities, as well as in those with elevated fibrosis-4 (FIB-4) index scores.3 HCV also increases risk of more advanced liver disease.4 Cirrhosis increases mortality risk in patients, particularly in those with MASLD and a BMI under 25.5
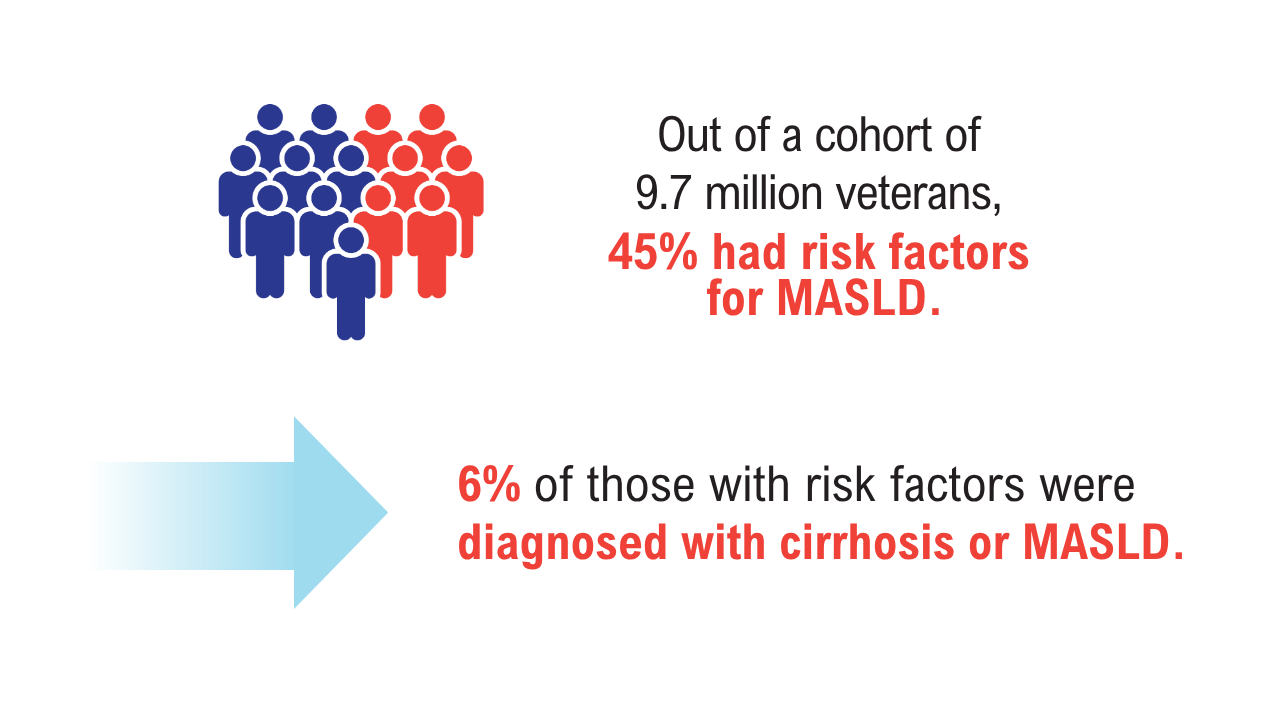 MASLD in At-Risk Veterans1
MASLD in At-Risk Veterans1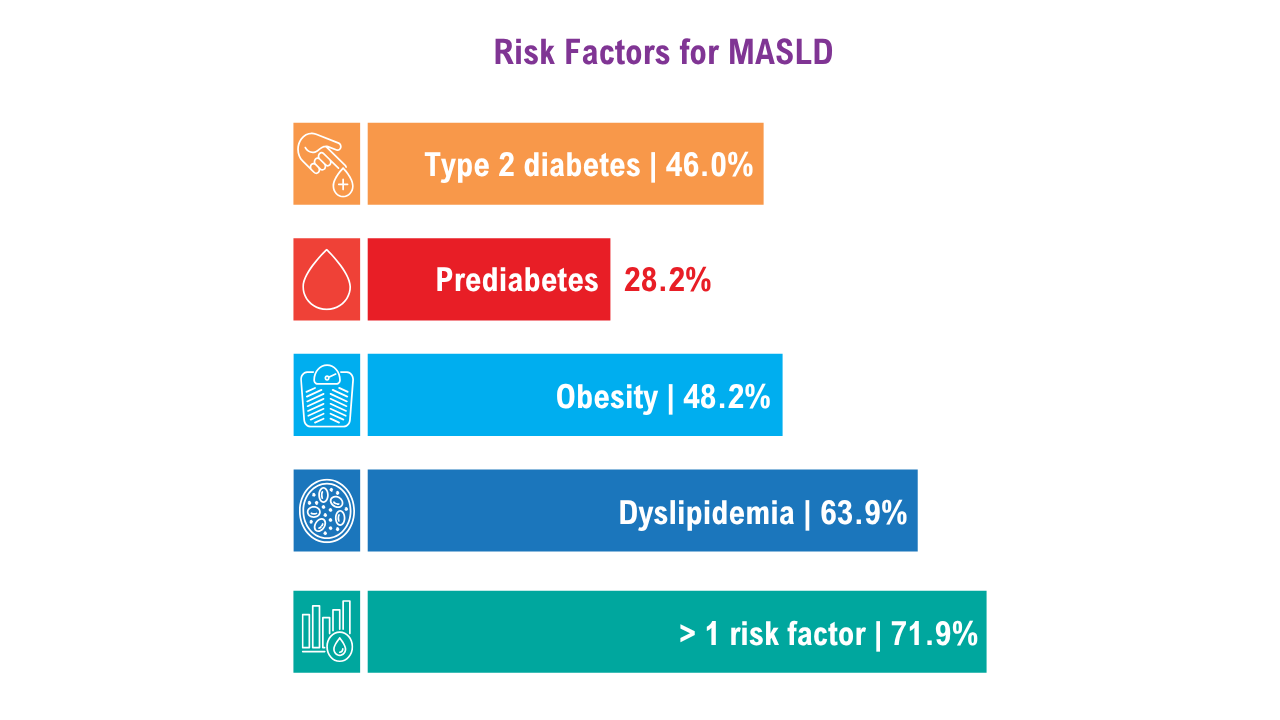 MASLD in At-Risk Veterans1More than half of the veterans with MASLD risk factors had FIB-4 scores that would prompt screening. Of those who were at risk, 9% received specialty care for liver disease, and 2% underwent elastography. Receiving a MASLD and cirrhosis diagnosis increased the odds of being seen by gastroenterology and hepatology clinicians by 5 and 8.3 times, respectively.
MASLD in At-Risk Veterans1More than half of the veterans with MASLD risk factors had FIB-4 scores that would prompt screening. Of those who were at risk, 9% received specialty care for liver disease, and 2% underwent elastography. Receiving a MASLD and cirrhosis diagnosis increased the odds of being seen by gastroenterology and hepatology clinicians by 5 and 8.3 times, respectively.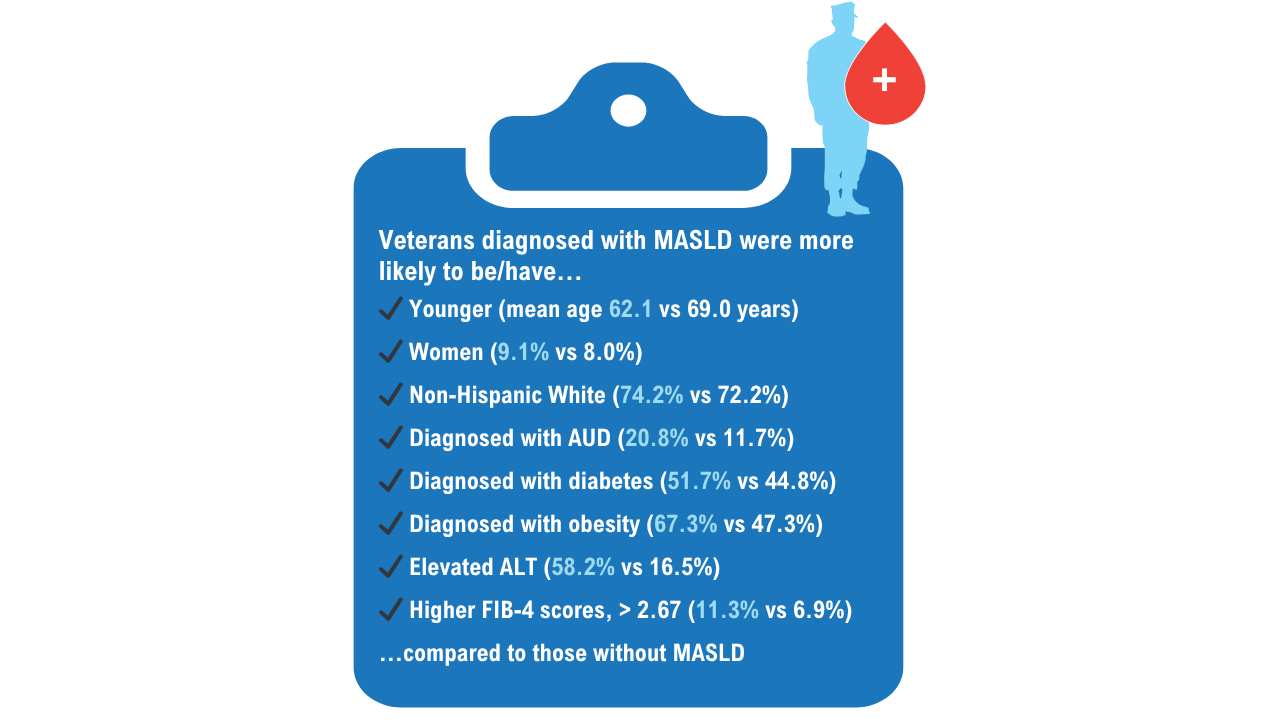 MASLD in At-Risk Veterans1
MASLD in At-Risk Veterans1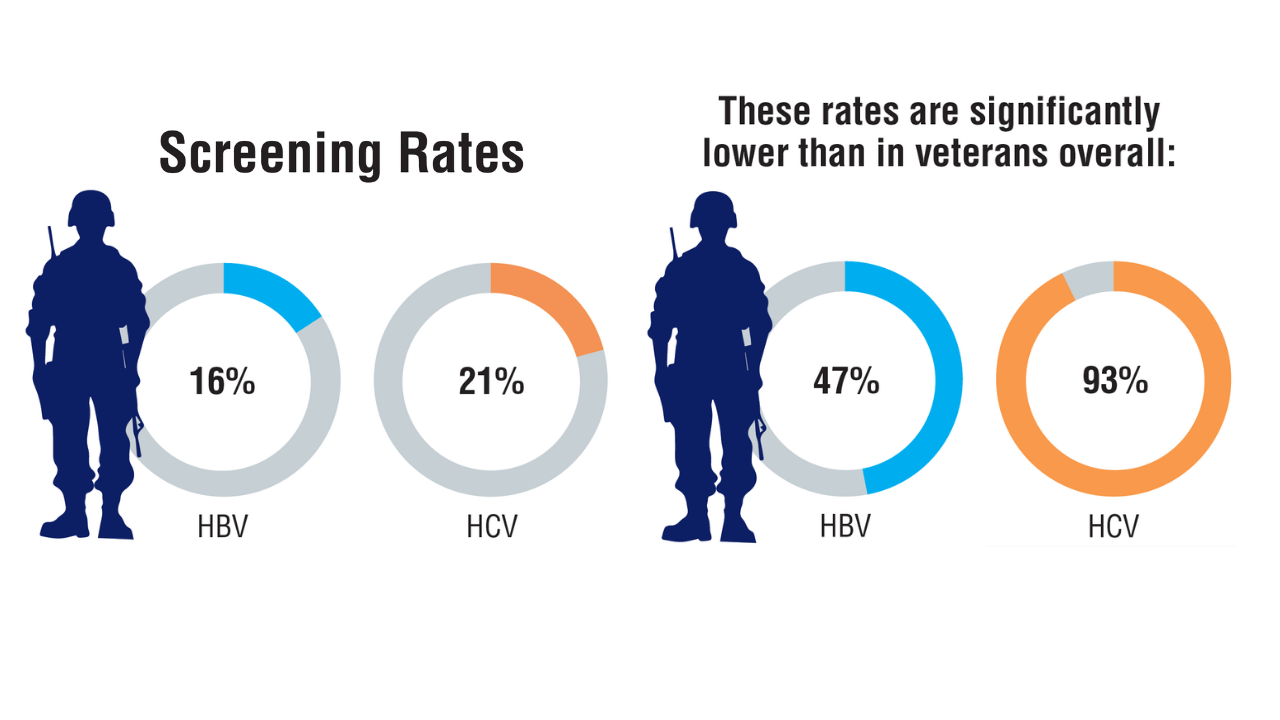 Viral Hepatitis Screening Rates in Low-Income Veterans2Lifetime HBV and HCV screening rates and associated factors were assessed among 933 low-income veterans. The results showed suboptimal screening, particularly for those with HBV, with notable disparities among veterans experiencing homelessness or extreme poverty.
Viral Hepatitis Screening Rates in Low-Income Veterans2Lifetime HBV and HCV screening rates and associated factors were assessed among 933 low-income veterans. The results showed suboptimal screening, particularly for those with HBV, with notable disparities among veterans experiencing homelessness or extreme poverty.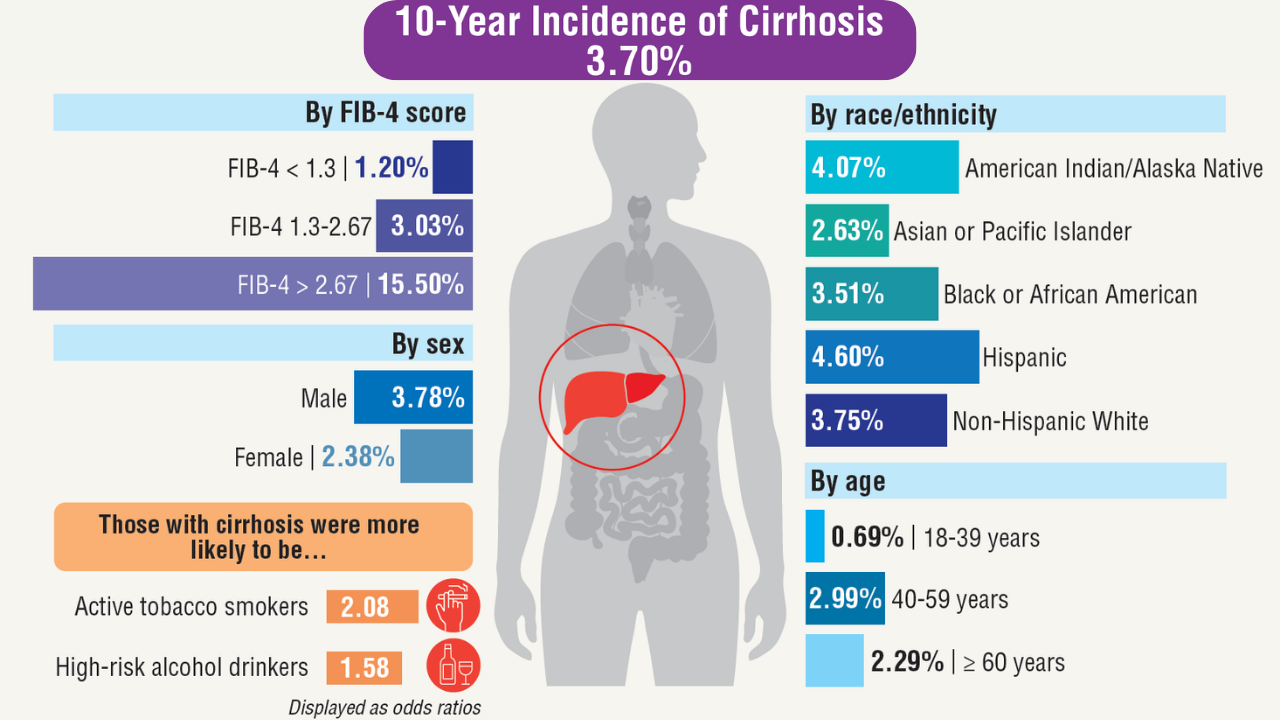 Incidence of Cirrhosis in Veterans With MASLD3
Incidence of Cirrhosis in Veterans With MASLD3
Nearly 1 million veterans with noncirrhotic MSLD were followed from 2010 to 2022 to assess future incidence of cirrhosis.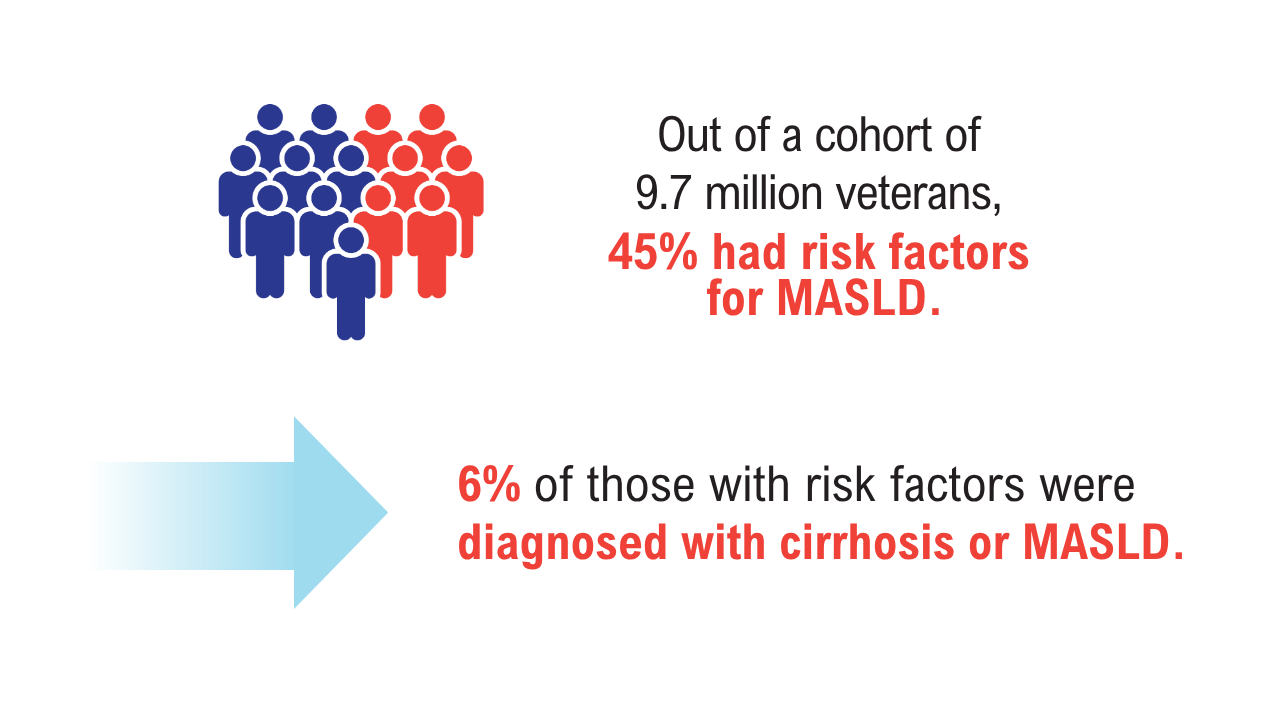 MASLD in At-Risk Veterans1
MASLD in At-Risk Veterans1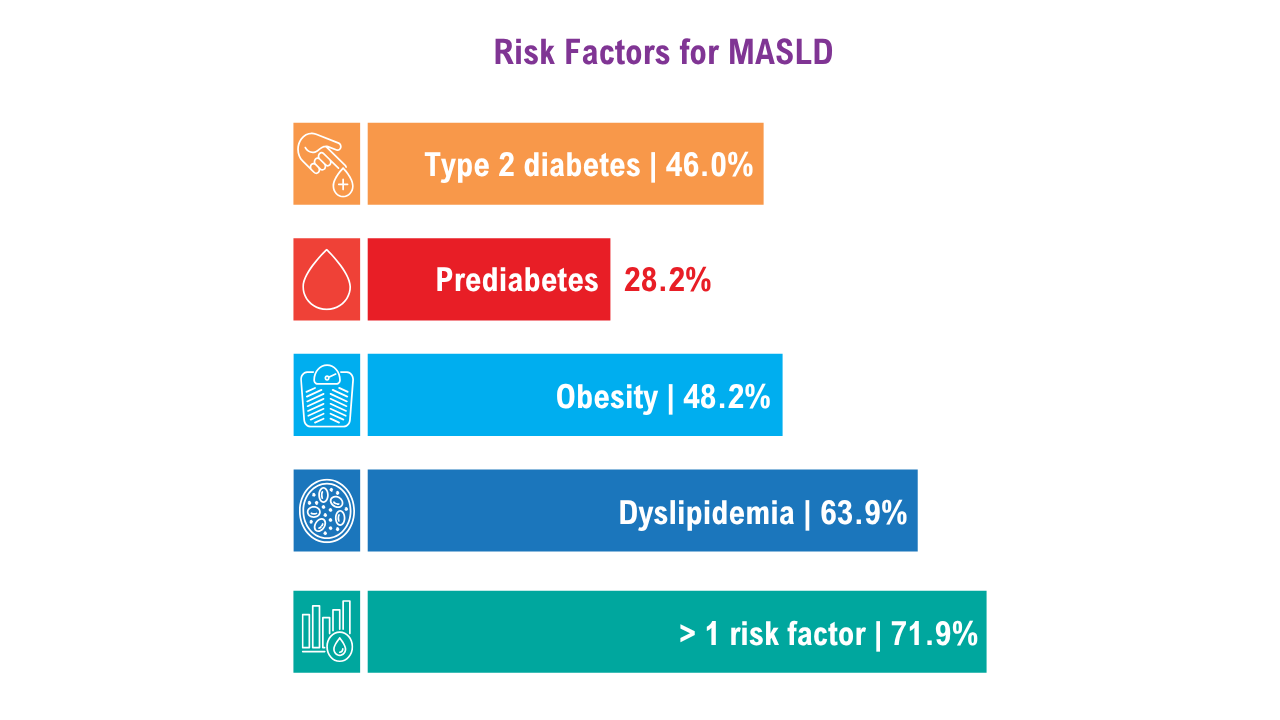 MASLD in At-Risk Veterans1More than half of the veterans with MASLD risk factors had FIB-4 scores that would prompt screening. Of those who were at risk, 9% received specialty care for liver disease, and 2% underwent elastography. Receiving a MASLD and cirrhosis diagnosis increased the odds of being seen by gastroenterology and hepatology clinicians by 5 and 8.3 times, respectively.
MASLD in At-Risk Veterans1More than half of the veterans with MASLD risk factors had FIB-4 scores that would prompt screening. Of those who were at risk, 9% received specialty care for liver disease, and 2% underwent elastography. Receiving a MASLD and cirrhosis diagnosis increased the odds of being seen by gastroenterology and hepatology clinicians by 5 and 8.3 times, respectively.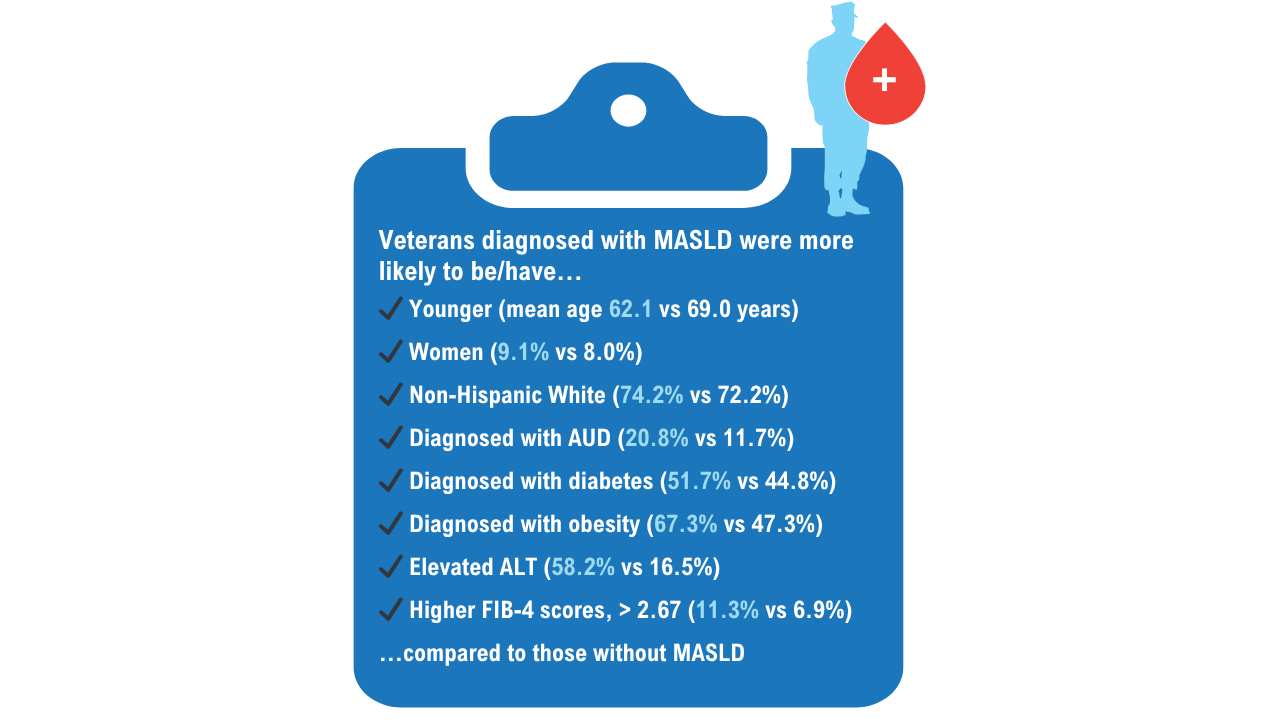 MASLD in At-Risk Veterans1
MASLD in At-Risk Veterans1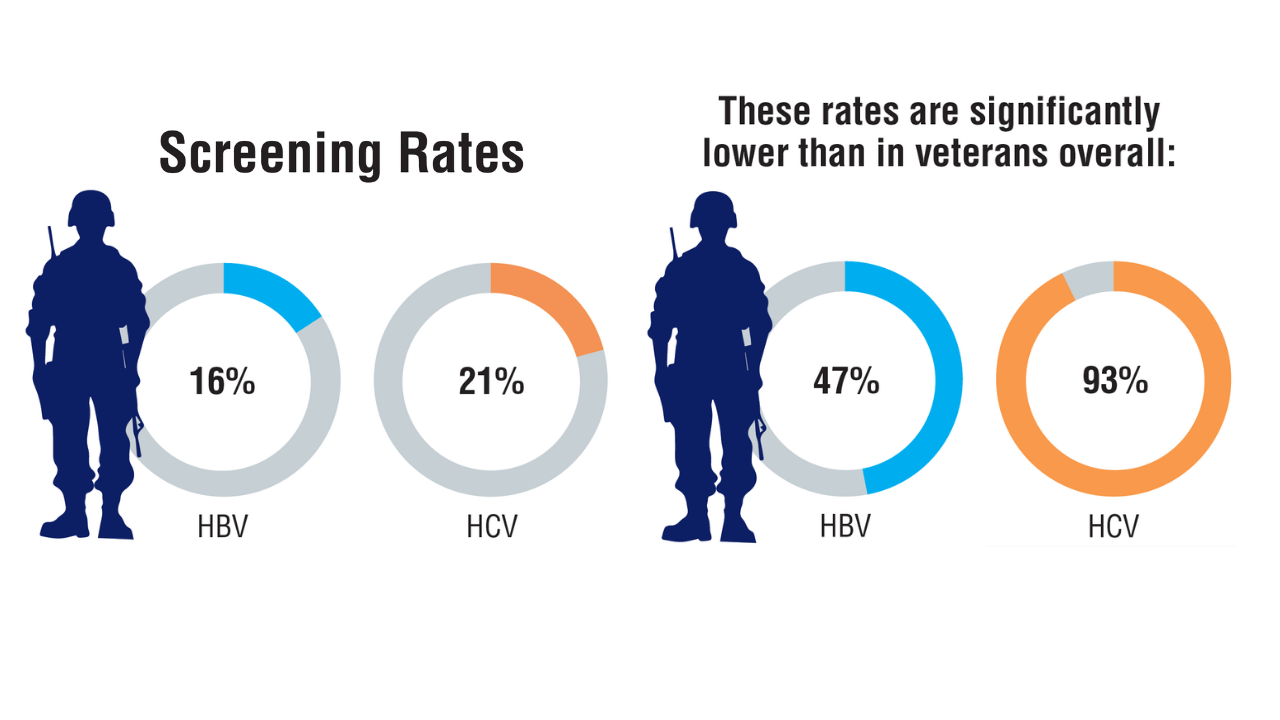 Viral Hepatitis Screening Rates in Low-Income Veterans2Lifetime HBV and HCV screening rates and associated factors were assessed among 933 low-income veterans. The results showed suboptimal screening, particularly for those with HBV, with notable disparities among veterans experiencing homelessness or extreme poverty.
Viral Hepatitis Screening Rates in Low-Income Veterans2Lifetime HBV and HCV screening rates and associated factors were assessed among 933 low-income veterans. The results showed suboptimal screening, particularly for those with HBV, with notable disparities among veterans experiencing homelessness or extreme poverty.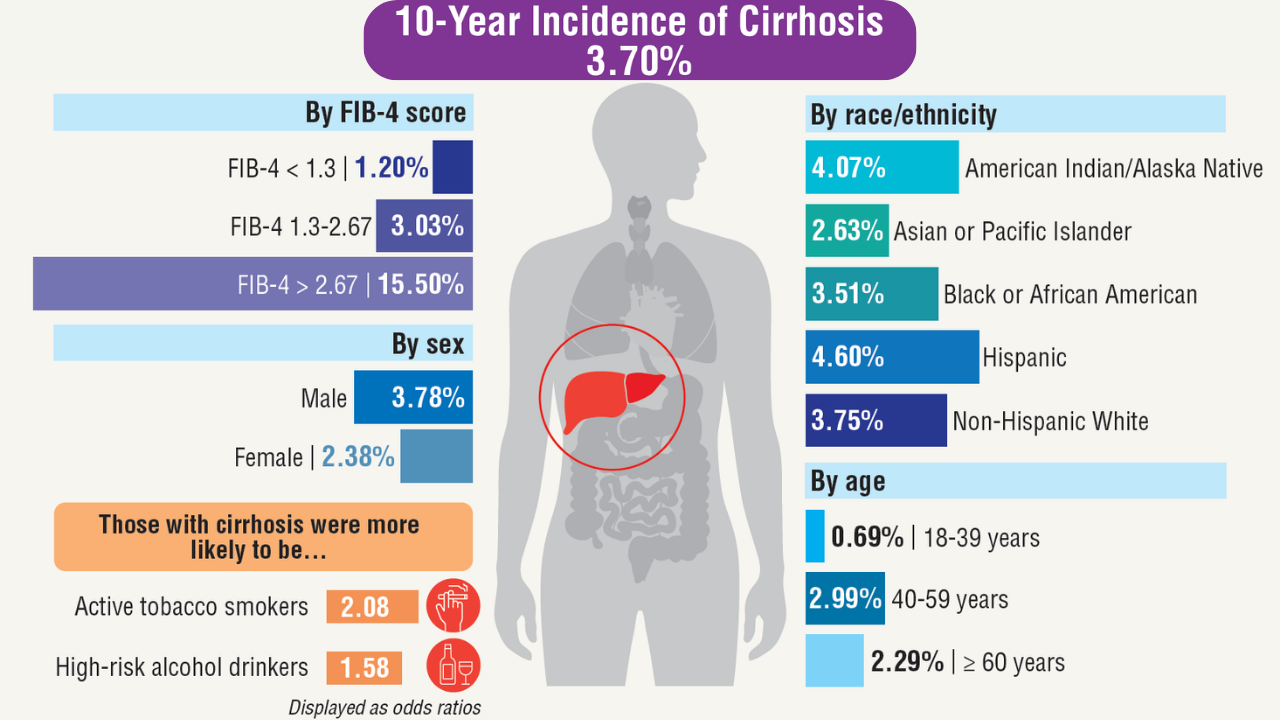 Incidence of Cirrhosis in Veterans With MASLD3
Incidence of Cirrhosis in Veterans With MASLD3
Nearly 1 million veterans with noncirrhotic MSLD were followed from 2010 to 2022 to assess future incidence of cirrhosis.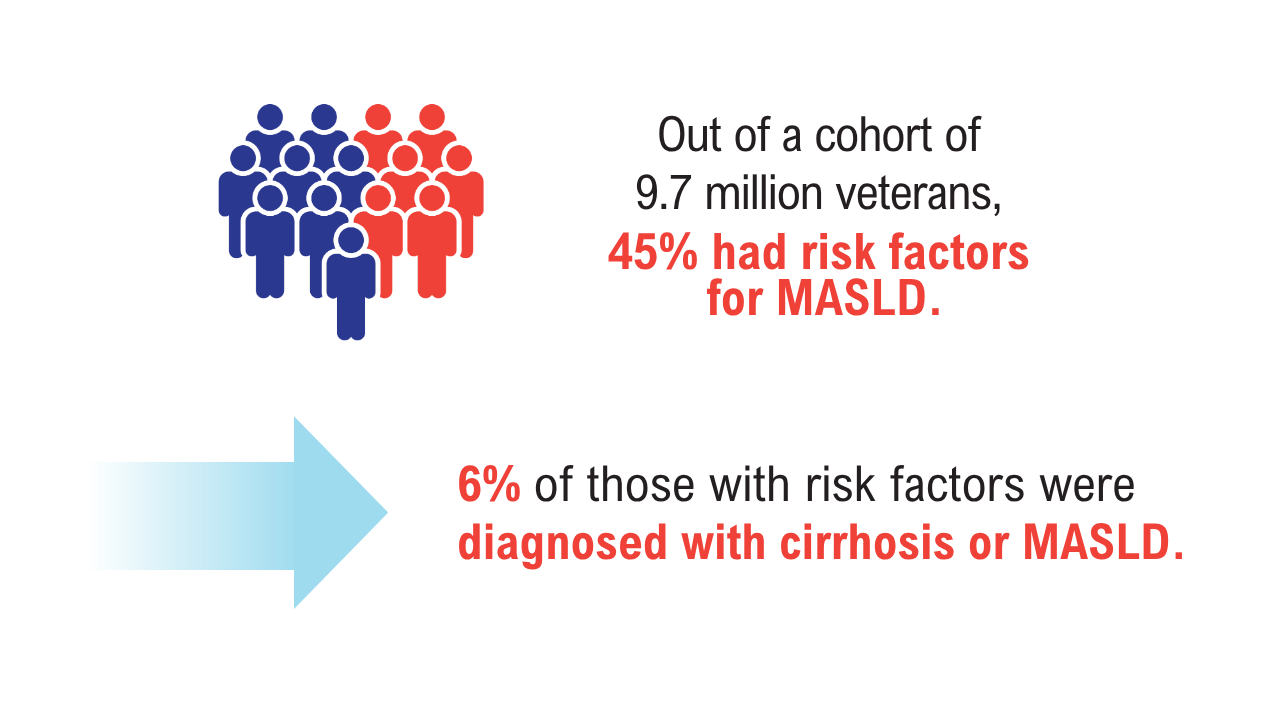 MASLD in At-Risk Veterans1
MASLD in At-Risk Veterans1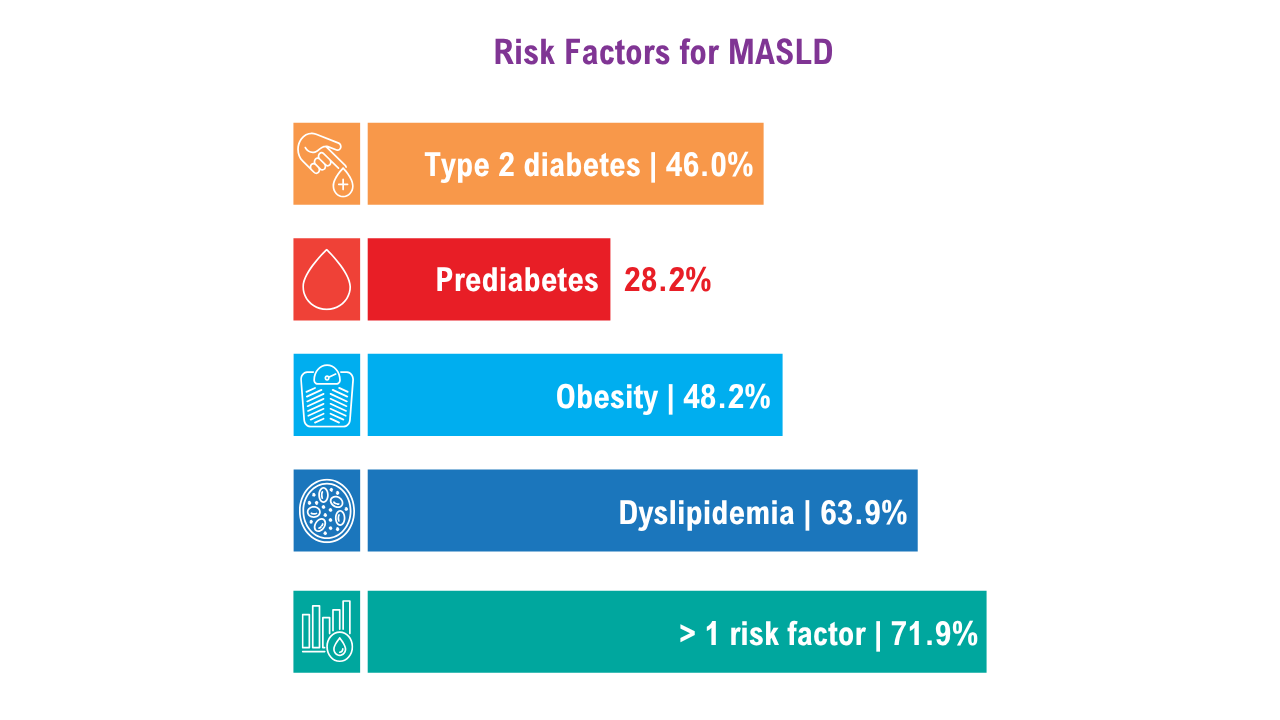 MASLD in At-Risk Veterans1More than half of the veterans with MASLD risk factors had FIB-4 scores that would prompt screening. Of those who were at risk, 9% received specialty care for liver disease, and 2% underwent elastography. Receiving a MASLD and cirrhosis diagnosis increased the odds of being seen by gastroenterology and hepatology clinicians by 5 and 8.3 times, respectively.
MASLD in At-Risk Veterans1More than half of the veterans with MASLD risk factors had FIB-4 scores that would prompt screening. Of those who were at risk, 9% received specialty care for liver disease, and 2% underwent elastography. Receiving a MASLD and cirrhosis diagnosis increased the odds of being seen by gastroenterology and hepatology clinicians by 5 and 8.3 times, respectively.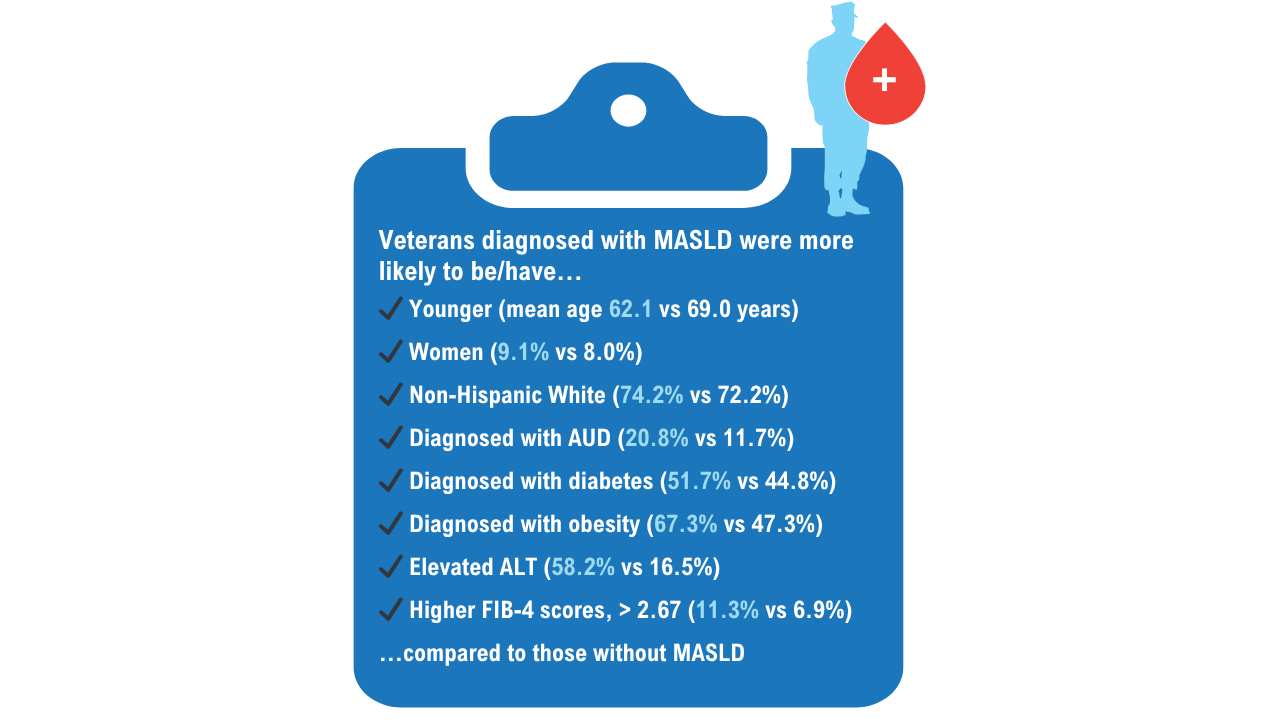 MASLD in At-Risk Veterans1
MASLD in At-Risk Veterans1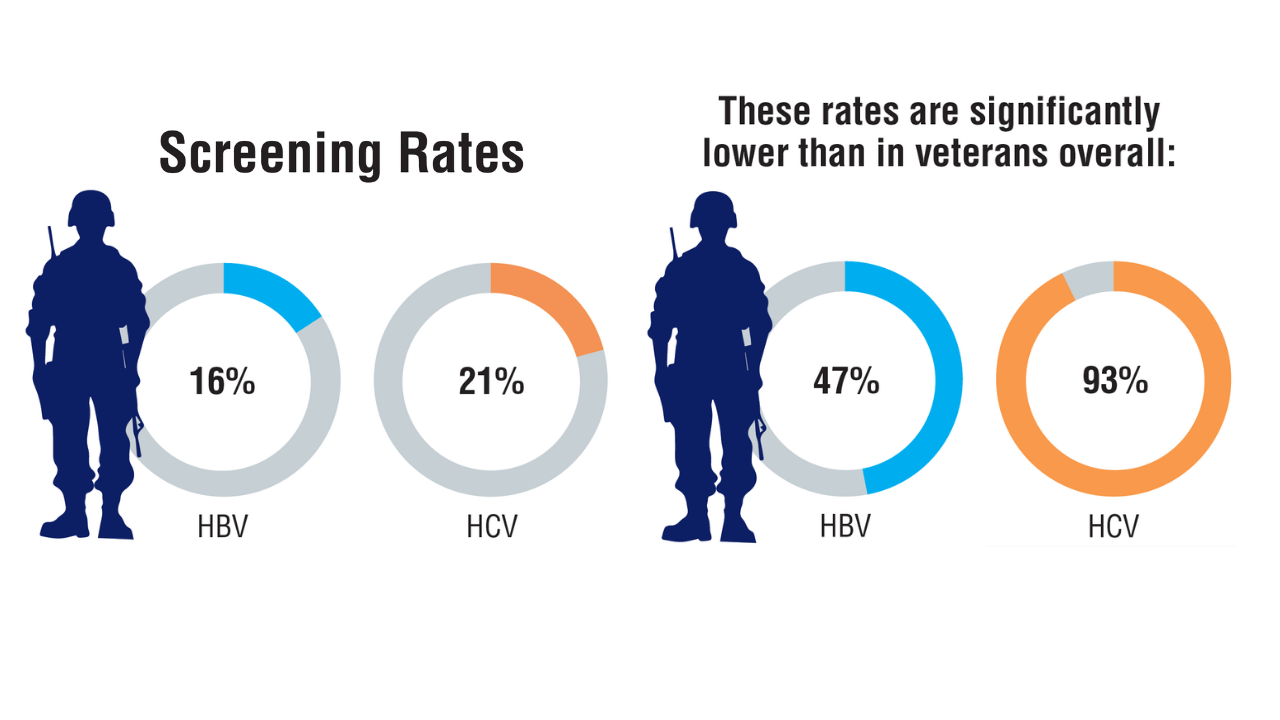 Viral Hepatitis Screening Rates in Low-Income Veterans2Lifetime HBV and HCV screening rates and associated factors were assessed among 933 low-income veterans. The results showed suboptimal screening, particularly for those with HBV, with notable disparities among veterans experiencing homelessness or extreme poverty.
Viral Hepatitis Screening Rates in Low-Income Veterans2Lifetime HBV and HCV screening rates and associated factors were assessed among 933 low-income veterans. The results showed suboptimal screening, particularly for those with HBV, with notable disparities among veterans experiencing homelessness or extreme poverty.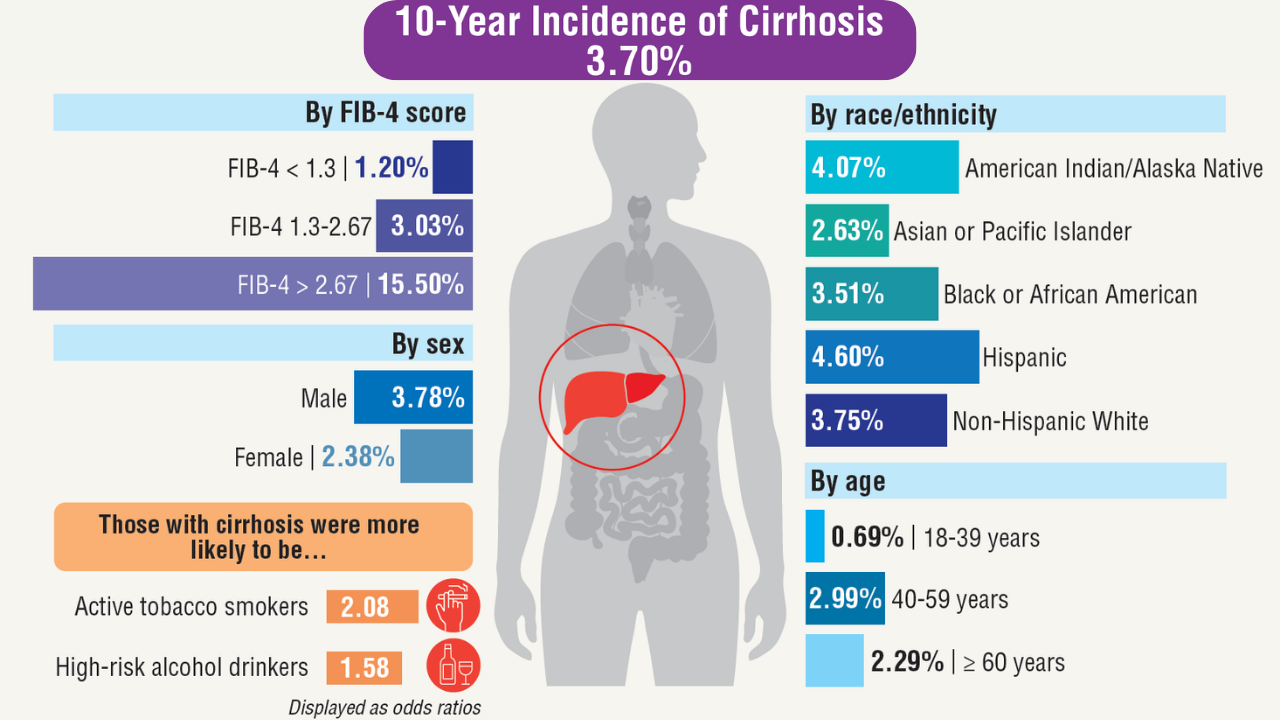 Incidence of Cirrhosis in Veterans With MASLD3
Incidence of Cirrhosis in Veterans With MASLD3
Nearly 1 million veterans with noncirrhotic MSLD were followed from 2010 to 2022 to assess future incidence of cirrhosis.
Click here to view more from Federal Health Care Data Trends 2025.
,false